The doctor's newspaper
OCTOBER 2025
Primary care goes digital
As technology continues to advance, its integration into primary care promises to not only address current challenges but pave the way for a more equitable, efficient, and patient-centred


R UNBEN PILLAY, CO-CHAIR of the Africa Telehealth Collaboration, took centre stage at the recent Health Funders Association Scenario Planning Symposium, where thought leaders gathered to envision Healthcare 2030: Building a Health System We Deserve. His presentation highlighted the transformative power of digital technologies in primary care, painting a compelling vision of how innovation can address systemic challenges, improve patient outcomes, and create a more sustainable healthcare model.
The session, co-facilitated by Jeremy Yatt, CEO of Fedhealth, brought attention to pressing issues in healthcare and the critical role technology must play. Dr Pillay’s insights provided valuable guidance for practitioners, funders, and policymakers aiming to navigate this fast-evolving landscape.

THE IMPERATIVE FOR TRANSFORMATION
The complexity of modern healthcare means innovation

is no longer optional; it’s essential, Dr Pillay explained. With the world facing a shortage of healthcare professionals and the increasing prevalence of multi-morbidity, the limitations of traditional approaches have become evident. The unsustainable pressure placed on primary care systems necessitates the adoption of digital tools capable of improving access, efficiency, and outcomes.
Dr Pillay stressed that producing more health professionals alone cannot solve the growing demand. Instead, leveraging digital technologies offers a way to address these challenges through smarter workflows, enhanced patient engagement, and costeffective solutions.
DRIVING INNOVATION IN PRIMARY CARE
Dr Pillay shared an array of groundbreaking tools and practices reshaping primary care, underscoring that the pandemic acted as a catalyst for much-needed change. Below are the key pillars driving this transformation: 1. Telemedicine’s revolutionary impact “Telemedicine is probably one of the easiest
ways that we can increase access to care if we build and design it properly,” said Dr Pillay. The Covid-19 pandemic normalised the adoption of telemedicine worldwide. In primary care, telehealth platforms have enabled patients to access services remotely, which is particularly effective in managing chronic conditions, providing follow-up consultations, and enhancing accessibility in rural regions. However, barriers such as payment parity for teleconsultations, the need for regulatory frameworks, and funder buy-in remain critical in expanding telehealth's reach.
“The interesting thing is that we're doing a lot of telemedicine in the private sector and maybe in the general practitioner space in the slightly uninsured space. And I think in the public sector, this is the biggest opportunity of increase in access to care. And there needs to be a bigger drive in the public sector for this to happen as well,” Dr Pillay said. 2. Empowering practices through electronic health records (EHRs) Despite its recognised advantages, EHR adoption in SA remains low, with only 20% of
general practitioners currently utilising such systems. Dr Pillay highlighted the untapped potential of EHRs in supporting value-based care by consolidating meaningful patient data and streamlining workflows.
More advanced EHR systems now incorporate AI capabilities, helping practitioners analyse data in real time and delivering actionable insights for better clinical outcomes. “The challenge is that as we move into this new age of value-based care and outcomes, we actually have to have EHR to know the data,” said Dr Pillay. “We're never going to get to that value-based care and outcomes unless all practitioners know what their data sets are, what their patient bases are, and the data currently sits with the funders, but as practitioners we need that EHR to sit in the practice on dashboards that we can see at any given time. We need to move all practitioners from paper-based practices into paperless practices.”
3. Leveraging mobile health (mHealth) Africa’s widespread mobile penetration creates a unique opportunity for mHealth solutions.



• Effective protection against MenB from 2 months of age1,3
• Administered in a 2- or 3-dose series1
• Can be given concomitantly with most routine childhood vaccines^1
• Available in a convenient pre-filled syringe with 2 needles1
Recommend. Repeat. Reinforce. Remember. Recommend BEXSERO to all your eligible patients ≥2 months of age today1
As with all injectable vaccines, appropriate medical treatment and supervision should always be readily available in case of an anaphylactic event following vaccination. Anxiety-related reactions (syncope, hyperventilation) may occur. It is important that procedures are in place to avoid injury from fainting. Not all recipients will be protected; 4CMenB vaccine does not cover all MenB strains. Fever risk in infants <2 years; prophylactic antipyretics recommended as per local guidelines. Immunocompromised individuals may have reduced immune response. Eculizumab users remain at risk for MenB despite vaccination. Not established for individuals >50 years and limited data in chronic conditions. Premature infants (≤28 weeks) may require 48-72h respiratory monitoring post-vaccination. Latex sensitivity: No natural rubber latex detected, but safety not confirmed. Kanamycin sensitivity: Trace amounts (<0.01 mcg/dose); safety not confirmed. PREGNANCY & LACTATION: Insufficient clinical data on exposed pregnancies are available. Information on the safety of the vaccine to women and their children during breast-feeding is not available. The benefit-risk ratio must be examined before making the decision to immunise during breast-feeding.

Platforms like WhatsApp can facilitate patient-practitioner interactions, real-time updates, and enhanced self-care measures. These tools not only make healthcare more accessible but also empower patients to take an active role in managing their health.
THE POTENTIAL OF WEARABLES AND AI TOOLS
Dr Pillay drew attention to the growing role of wearable devices and AI-powered diagnostics in reshaping traditional care models. Smartwatches, oximeters, and advanced diagnostic technologies are enabling earlier detection and proactive management of chronic conditions like diabetes and cardiac irregularities. In addition, ‘hospital-at-home’ systems, which integrate remote monitoring devices, are proving that quality acute care can be delivered outside traditional hospital settings. This redefines patient care by reducing hospital stays and long-term costs. AI is also pushing boundaries in diagnosis and precision care. From early detection of diabetic retinopathy to identifying cardiac irregularities without immediate specialist intervention, AI tools are providing equal opportunities for quality care across varying healthcare settings. By lowering referral rates and enhancing real-time decision-making, AI
proves indispensable in optimising resource-limited regions.
TRANSFORMING MENTAL HEALTH SERVICES
With the global mental health crisis escalating, digital therapeutics and mobile apps offer new hope. These scalable solutions provide psychological support in areas lacking adequate access to psychologists or psychiatrists. By integrating mental healthcare into digital platforms, practitioners can expand their reach, ensuring patients receive timely assistance.
COLLABORATION: THE KEY TO SUCCESS
Dr Pillay outlined a vision of digital transformation anchored by collaboration among healthcare practitioners, funders, and technology developers. He called for:
• Interoperability: Systems that integrate seamlessly across fragmented healthcare networks
• Education and training: Practitioners need robust education to bridge technological gaps and inspire confidence in adopting digital solutions
• Sustainable funding models: Reimbursement structures must evolve to accommodate advancements such as
Transforming care, preserving humanity
DEAR READER
This October 2025 issue of Medical Chronicle stands as a testament to the remarkable convergence of innovation, clinical excellence, and patient-centred care that defines medicine.
In our cover feature, ‘Primary care goes digital’, Dr Unben Pillay guides us through the revolutionary changes reshaping healthcare delivery across South Africa. This comprehensive exploration demonstrates how telemedicine, electronic health records, and AI-driven diagnostics are not merely technological add-ons, but fundamental tools for enhancing accessibility and outcomes. In infectious diseases, we present a review of invasive meningococcal disease, providing crucial epidemiological data and treatment strategies that could prove lifesaving in your practice. This issue tackles some of healthcare’s most pressing concerns with characteristic rigour. Prof Morgan Chetty’s thought-provoking piece on ‘The patient journey’ challenges us

to reimagine healthcare delivery through a truly patient-centric lens. Meanwhile, our exploration of obesity as malnutrition offers fresh perspectives on this global epidemic, connecting lifestyle interventions with Type 2 diabetes prevention in ways that will resonate with practitioners across all specialties.
The psychiatric section presents groundbreaking insights into addiction treatment, including Dr Kobus Roux’s fascinating webinar report on ‘The addicted brain’. These articles illuminate the neurobiological foundations of addiction while offering practical approaches for building resilience during challenging times.
As we progress through 2025, the themes emerging in this issue –technological integration, patient-centred care, interdisciplinary collaboration, and evidence-based innovation – will continue to define excellence in healthcare delivery. The case studies and realworld applications featured throughout these pages provide not just theoretical knowledge, but practical tools you can implement immediately.
We hope this issue serves as both a comprehensive clinical resource and an inspiration for the continued advancement of healthcare in South Africa and beyond. Your dedication to lifelong learning and patient care remains the cornerstone of medical progress.
Happy reading.

telemedicine, AI diagnostics, and wearables, ensuring digital integration is economically viable. Healthcare transformation, Dr Pillay emphasised, is not solely a technological pursuit but an ecosystem-level change requiring alignment across stakeholders.
A CALL TO ACTION
Dr Pillay concluded with a compelling call to action: Digital transformation is no longer an aspiration – it is an imperative. He encouraged decision-makers to embrace technology as the cornerstone for a sustainable future in primary care.
The integration of digital innovations, he argued, can foster health equity, improve
efficiency, and ensure that healthcare systems are better prepared to meet the demands of tomorrow’s patients.
Dr Pillay’s presentation at the Health Funders Association Symposium resonated as a powerful message of hope and progress. As technology continues to advance, its integration into primary care promises to not only address current challenges but pave the way for a more equitable, efficient, and patient-centred healthcare system.
By prioritising innovation and cross-sector collaboration, stakeholders can realise Dr Pillay’s vision of building a health system we deserve.

May reduce pain and stiffness
May improve joint function
Once a day dosage
Starts working from 5 days



Mediterranean diet a shield against Alzheimer’s?
New study shows diet could reduce genetic dementia risk, even in high-risk individuals.
By Nicky Belseck, medical journalist
RECENT RESEARCH PUBLISHED in Nature
Medicine provides compelling evidence suggesting that the Mediterranean diet (MedDiet) may serve as a powerful tool in reducing the risk of Alzheimer's disease (AD) and related dementias (AD/ADRD), even among individuals with a genetic predisposition to the condition.
The study, which analysed data from over 5 700 individuals, examined interactions between genetics –including the high-risk APOE4 genotype – metabolic markers, and adherence to a Mediterranean dietary pattern. The findings hold important implications for medical professionals focused on dementia prevention and tailored nutritional interventions.
GENETIC RISK AND THE MODIFYING ROLE OF DIET
The APOE4 genotype is one of the strongest known genetic factors contributing to Alzheimer's disease. However, the study revealed that adherence to a MedDiet – characterised by foods like fruits, vegetables, nuts, whole grains, fish, and olive oil – can significantly lower the risk of dementia, even for those carrying two copies of the APOE4 allele (homozygotes).
A key aspect of the research was examining 57 specific blood plasma metabolites associated with either increased or decreased AD risk. In APOE4 carriers, certain lipid-derived metabolites, such as cholesteryl esters and sphingomyelins, were associated with a heightened risk of dementia. However, the study also highlighted that adherence to the MedDiet was linked to lower levels of these harmful metabolites. Even more promising, higher intake of the MedDiet appeared to reverse this metabolite-related risk specifically in APOE4 homozygotes.
This groundbreaking finding suggests that diet could mitigate some of the genetic risk factors, offering a preventative strategy for high-risk patients.
PRECISION NUTRITION: A NEW FRONTIER?
The study went further to explore causal relationships
between metabolites and cognitive decline using Mendelian randomisation. Nineteen metabolites were identified as having a direct role in influencing dementia and cognitive outcomes, paving the way for precision nutrition approaches designed to target individual metabolic profiles.
Interestingly, the research also demonstrated that incorporating metabolomic data into dementia risk prediction models improved accuracy, especially in the early stages when proactive interventions are most effective. This presents an opportunity for clinicians to integrate dietary recommendations with genetic and metabolic profiling for personalised prevention strategies.
IMPLICATIONS FOR CLINICAL PRACTICE
For physicians, the implications of this research are clear: promoting the Mediterranean diet could be a cost-effective, accessible preventative measure to combat Alzheimer's disease. Given the strong synergy observed between diet and genetic risk, early adoption of this dietary pattern may be critical for patients with known genetic susceptibilities.
This study adds to the growing body of evidence supporting the benefits of the Mediterranean diet not only for cardiovascular and metabolic health but also for long-term brain health. Physicians are encouraged to actively discuss dietary habits with patients at risk of cognitive decline and work toward sustainable dietary interventions tailored to individual genetic profiles. In conclusion, while genetic predisposition plays an outsized role in Alzheimer's disease, this research underscores the power of lifestyle interventions – particularly the Mediterranean diet – to offset genetic risks, marking a turning point in how we approach dementia prevention.
Source: Liu Y, Gu X, Li Y. et al. Interplay of genetic predisposition, plasma metabolome and Mediterranean diet in dementia risk and cognitive function. Nat Med. August 2025. Available from: https://doi.org/10.1038/s41591025-03891-5

Why gender and social equity matter in the fight against AMR

By
NTIMICROBIAL RESISTANCE
(AMR) poses one of the most pressing global health challenges of the 21st century. As the World Health Organization revises the Global Action Plan (GAP) on AMR for completion in 20252026, healthcare professionals have an opportunity to address long-standing inequities that exacerbate this crisis. The revised GAP emphasises equity and gender responsiveness across its strategies, aiming to create a people-centred, inclusive framework for combating AMR.
THE ROLE OF GENDER AND EQUITY IN AMR
AMR vulnerabilities are deeply influenced by gender, socioeconomic status, and cultural norms. Women in low-resource settings often face disproportionate risks due to caregiving roles and limited access to healthcare. Additionally, marginalised populations, such as older adults, persons with disabilities, and migrant communities, experience barriers in accessing essential healthcare, clean water, and hygiene resources – factors that escalate infection risks and misuse of antimicrobials. Biases in antibiotic prescribing also play a role. Inaccessible healthcare, reliance on informal providers, and cultural stigmas drive overuse and misuse of antimicrobials, contributing to resistance. Addressing these inequities is key to developing sustainable and effective AMR interventions.
INTEGRATING
EQUITY INTO AMR STRATEGIES
The revised GAP incorporates equityfocused principles across its five strategic pillars: awareness, surveillance, infection prevention, antimicrobial stewardship, and governance. For healthcare providers, this means being at the forefront of ensuring equitable access to AMR interventions at every stage:
1. Education as a transformative tool: Awareness campaigns must resonate with diverse populations, addressing cultural and gender-specific needs. Healthcare
professionals can work with grassroots organisations to create inclusive materials and tools that empower communities to change harmful practices.
2. Enhanced surveillance systems: Current AMR surveillance often omits vital demographic data, such as gender, geography, or socioeconomic status. Incorporating these markers will paint a clearer picture of how AMR impacts underserved populations. This requires healthcare professionals to advocate for inclusive research and the equitable sharing of anonymised data.
3. Improved access to preventative measures: Limited water, sanitation, and hygiene (WASH) resources leave vulnerable populations at higher infection risks. Doctors and health advocates can push for policies that ensure access to WASH infrastructure and vaccination programmes, particularly in disadvantaged regions.
4. Equity in antimicrobial usage: Reducing prescribing biases and establishing stewardship programmes that target underserved populations is essential. Training healthcare providers about unconscious biases and enabling fair access to antimicrobials will help optimise practices.
5. Inclusive governance structures: Diverse representation, including gender equity specialists and marginalised community advocates, is vital in decisionmaking. Healthcare professionals must influence the creation of national AMR strategies that reflect the voices and needs of these populations.
HEALTHCARE’S ROLE IN AMPLIFYING EQUITY
Healthcare professionals are uniquely positioned to champion equitable AMR strategies. This includes advocating for better research funding, inclusive policymaking, and the development of
people-centred interventions. Emphasising equity ensures that AMR policies not only protect marginalised communities but also contribute to the resilience of health systems worldwide.
The revised Global Action Plan on AMR provides an opportunity to address systemic inequities in healthcare. By integrating gender and equity considerations, healthcare professionals can drive impactful change, protect vulnerable populations,
and ensure that AMR strategies remain inclusive and effective in combating resistance globally.
SOURCE: Batheja D, Saint V, Dobreva Z, et al. Integrating gender and equity commitments in the revised global action plan on antimicrobial resistance. The Lancet. September 2025. Available from: https://www.thelancet.com/journals/ lancet/article/PIIS0140-6736(25)01377-7/ fulltext?dgcid=raven_jbs_etoc_email




HASA Conference 2025: Sustainable healthcare together
UNDER THE THEME ‘Sustainable Healthcare Together’, the conference focused on advancing resilience, collaboration, and technological innovation in SA's healthcare landscape. Leading hospital groups such as Netcare, Mediclinic, and Life Healthcare participated alongside independent facilities.
KEY THEMES AND SESSIONS
Doctors, policymakers, and healthcare leaders engaged deeply on:
• Innovation in healthcare: Discussions on implementing AI, robotics, and telemedicine in clinical practice
• Sustainable health systems: Addressing future-proofing and systemic efficiencies
• Policy reform insights: Alternatives to National Health Insurance (NHI) and private healthcare funding strategies
• Clinical quality improvements: Reducing medical errors and personalising care for better outcomes.
The event included notable sessions such as the Health Leadership Panel, and presentations on AI applications in medical fields like cardiovascular health and patient monitoring.
HIGHLIGHTED COLLABORATIONS
The conference proved a networking hotspot, hosting major international and local healthcare experts, with a concurrent technology exhibition featuring innovations like TeleICU and robotics-led patient care. Doctors also had opportunities to engage through panel discussions, abstract presentations, and a gala dinner.
WHY IT MATTERS
This flagship event is an essential platform for driving systemic reforms and harnessing innovation to secure sustainable and equitable healthcare in SA. For doctors, it provided firsthand insights into strategies for improving clinical outcomes amidst evolving challenges.









South Africans with obesity are malnourished, at high risk of T2DM
National Nutrition Week (9–15 October) highlighted the urgent need for better nutrition to combat South Africa’s skyrocketing rates of obesity and Type 2 diabetes. Many South Africans living with obesity, including children, are in fact malnourished, revealing a paradox at the heart of a worsening national health crisis.
BESITY IS A major risk factor for Type 2 diabetes, which occurs when the body’s insulin is insufficient or not
functioning properly. Both often coexist with other chronic conditions, including high blood pressure, heart disease and cancer.
EPCLUSA® is indicated for the treatment of chronic hepatitis C infection irrespective of genotype in treatment naïve or treatment experienced patients aged 12 years and older and weighing at least 30 kg:
- without cirrhosis or with compensated cirrhosis
- with decompensated cirrhosis in combination with ribavirin 1
Jana Retief, foundation manager at the non-profit The Noakes Foundation, says, “Obesity is seldom a failure of individual
Proven cure ratec: 98,9 % in real-world analysis2,3
Suitable for patients with various levels of liver disease severityb,d 2,3

Pan-genotypic and pan-fibroticb,d 3
1 tablet once daily, with or without food, for 12 weeks1
Footnotes: Despite unknowns in baseline characteristics of some patients, such as: HCV genotype, fibrosis stage, former/current IV drug use, PPI use at baseline and treatment history.3 bA large-cohort international real-world study showed that patients with unknown genotype (n = 42), unknown fibrosis score (n = 82) and unknown treatment history (n = 33) were cured with EPCLUSA® for 12 weeks. Cure is defined as SVR i.e., undetectable HCV RNA after treatment completion.3,4 cCases of HBV reactivation, some of them fatal, have been reported during or after treatment with direct acting antiviral agents including EPCLUSA®. HBV screening should be performed in all patients before initiation of treatment. Treatment with EPCLUSA® should not be initiated in patients who screened positive for hepatitis B virus infection. HBV/HCV coinfected patients are at risk of HBV reactivation, and should therefore be monitored and managed according to current clinical guidelines.1 dPatients with decompensated cirrhosis use EPCLUSA® + ribavirin for 12 weeks.1
Abbreviations: HCV = Hepatitis C Virus; RNA = Ribonucleic acid; IV = Intravenous; PPI = Proton pump inhibitor; SVR = Sustained virological response; HBV = Hepatitis B virus.
References: 1. Epclusa Professional Information approved by the medicine’s regulatory authority. 10 March 2022. 2. Lawitz E, Bourliere M, Han L, McNally J, Stamm LM, Brainard DM, et al. Treatment with SOF/VEL or SOF/VEL/VOX is well tolerated and results in high SVR12 in genotype 1-6 HCV-infected patients with minimal fibrosis: a retrospective analysis of the ASTRAL and POLARIS clinical studies. Poster THU-273 presented at the International Liver Congress 2017, April 19–21, Amsterdam, The Netherlands. Available at: https://www.natap.org/2017/EASL/EASL_07. htm [Accessed 24 March 2022]. 3. Mangia A, Milligan S, Khalili M, Fagiuoli S, Shafran SD, Carrat F, et al. Global real-world evidence of sofosbuvir/velpatasvir as simple, effective HCV treatment: Analysis of 5552 patients from 12 cohorts. Liver Int 2020;40:1841–1852. 4. National Guidelines for the Management of Viral Hepatitis. Department of Health Republic of South Africa Available at: https://sahivsoc.org/Files/SA%20NDOH_Viral%20Hepatitis%20guideilnes%20final_.pdf [Accessed 10 March 2022]. For full prescribing information refer to the professional information approved by the Medicines Regulatory Authority. S4 EPCLUSA® 400 mg/100 mg film-coated tablets. Reg. No.: 51/20.2.8/0872. Each film-coated tablet contains 400 mg sofosbuvir and 100 mg velpatasvir. For any adverse events, please contact: Safety_FC@gilead.com | EPCLUSA®, the EPCLUSA® Logo, GILEAD and the GILEAD Logo are trademarks of Gilead Sciences, Inc. or its related companies. All other trademarks referenced herein are the property of their respective owners. ©2025 Gilead Sciences, Inc. All rights reserved. Date of preparation: 04/2025 Job code: ZA-EPC-0022
48404 06/25
2025/06/27 09:06
willpower, and developing diabetes is rarely anyone’s fault. They are fuelled by today’s modern diet, characterised by increased consumption of sugar, refined carbohydrates and processed food, including fast food. Over the past 30 years, major shifts in South Africa’s food environment have led to poor nutrition.” Nutrition Week reminds us that eating better begins with understanding food.
“Nutrition interventions supported by rigorous scientific research and community-based nutrition education have sent a clear message: diets low in sugar and refined carbohydrates and rich in nutrient-dense whole foods improve blood sugar, support weight loss and can prevent, reverse or better manage Type 2 diabetes and related chronic diseases,” says Retief.
More than half of South Africa’s adult population is affected by obesity, and the country has one of the highest diabetes rates in Africa, where the disease is the second leading cause of death. Globally, one in four adults could be living with overweight and obesity by 2035, and one in eight with diabetes by 2050.
Obesityisseldom a failure of individual willpower,and developingdiabetes israrelyanyone’s fault
Retief explained, “In South Africa, dietitians often rotate between health facilities, and nutrition and lifestyle interventions are introduced too late, or not at all. This approach falls short of addressing the scale of the chronic illness threat. A coordinated response is essential, which is why we are proud to welcome multi-sectoral representatives to the event.”
Inspiring stories from Eat Better South Africa: The Noakes Foundation’s community-driven nutrition education programme, will also be featured. In Dunoon, near Cape Town, participants learned to identify hidden sugars, swap harmful foods for nourishing alternatives, read labels and prepare affordable, healthy meals. “Participants lost weight, lowered their blood sugar and blood pressure, improved key health markers and, most importantly, reclaimed their lives,” said Retief.
“True health isn’t just the absence of disease – it’s thriving in every aspect of life, supported by good nutrition and avoiding sugar, refined carbohydrates and processed foods,” concluded Retief.




How menopause restructures a woman's brain
New study links structural brain changes with cognitive, emotional, and physiological changes during menopause.
ANY WOMEN DURING menopause complain about brain fog, which includes symptoms like forgetfulness, trouble concentrating, and mental fatigue, often due to fluctuating hormone levels. A literature review was conducted to examine published studies that explore the link between structural brain changes
during menopause and cognitive, emotional and physiological outcomes. Menopause is associated with distinct structural changes in the brain. Multiple studies have documented reductions in grey matter volume in both the frontal and temporal cortices and the hippocampus–regions critical for memory and executive function.
These volumetric losses have been linked to declines in cognitive performance, particularly in verbal and visuospatial memory. Increased white matter hyperintensities have also been documented across multiple studies, especially among women with early menopause or those with frequent hot flashes. White matter
hyperintensities are bright spots seen on an MRI scan of the brain's white matter, often indicating damaged tissue typically due to reduced blood flow. These lesions can lead to neurological symptoms like cognitive decline, balance issues, and mood changes and are associated with an increased risk of stroke and dementia.
Some evidence suggestsapartial recoveryofgrey matter volume postmenopause, potentiallyreflecting compensatory neuroplastic processes
Discover how Altron HealthTech’s vision for simpler, safer, smarter healthcare became ThriveLink, a patient app enhancing cancer care through collaboration with providers and patients.



The Menopause Society. "These data will hopefully lead to a better understanding of the factors underlying some of the cognitive concerns experienced by women during the menopause transition so that we can ultimately identify effective therapies."
Source: www.menopause.org

Dr Peter Barrow
MBBCh (Wits); DCH (SA); FCP (SA); Cert. Gastro (SA)
Date: 22 October 2025
Time: 19h00
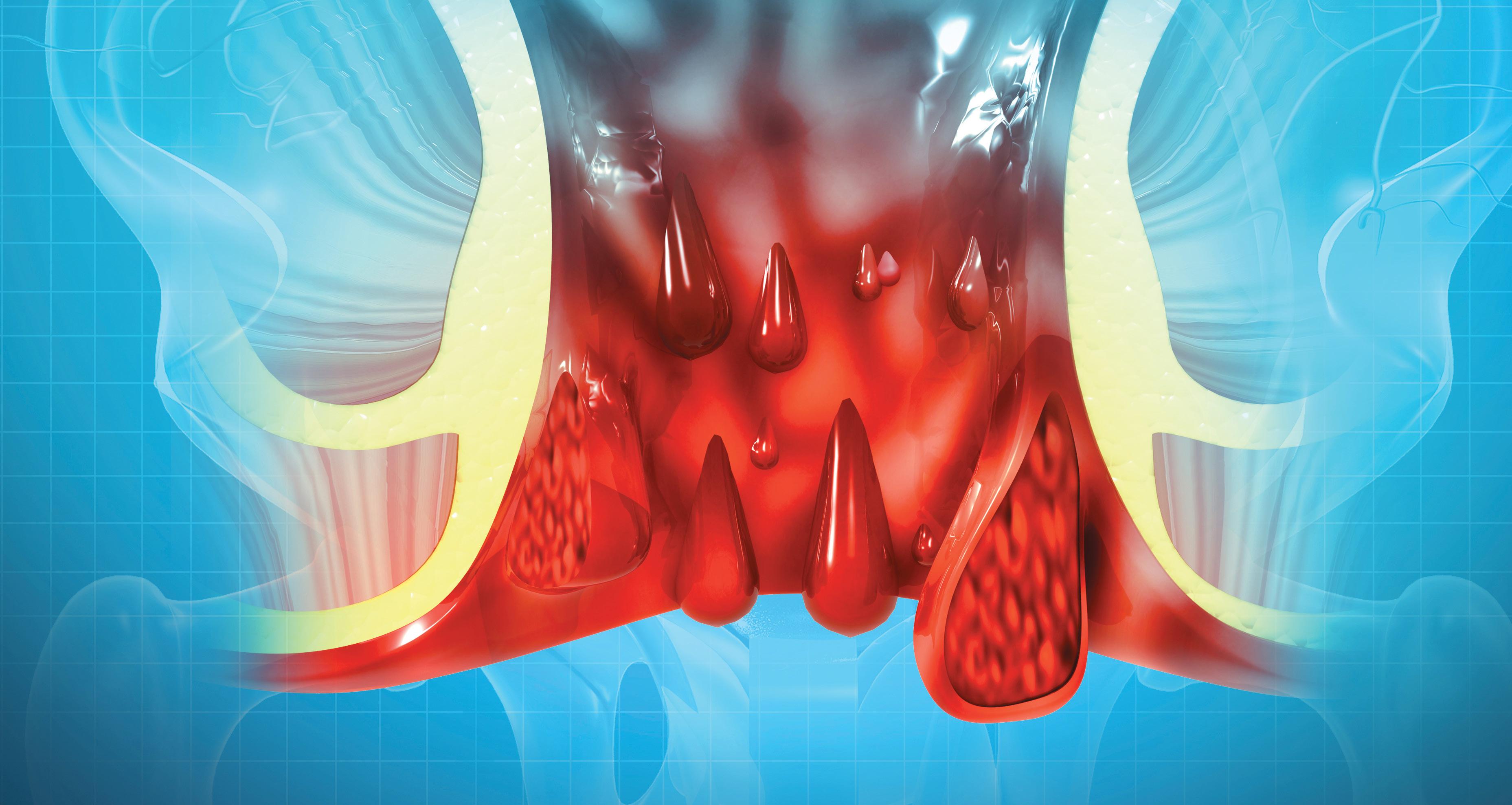
Topic: The bottom line on haemorrhoids: Latest updates & game changers
Speaker: Dr Peter Barrow
CLICK TO REGISTER: https://bit.ly/AcdocoWebinar22Oct25
Dr Barrow is a consultant gastroenterologist trained at the University of Witwatersrand, with a special interest in interventional endoscopy including double balloon endoscopy (DBE) and endoscopic ultrasound (EUS). He has extensive clinical and research experience in inflammatory bowel disease (ulcerative colitis and Crohn’s disease), coeliac disease, oesophageal motility disorders and GERD. He is a well recognised speaker and respected by his peers. Dr Barrow readily shares his practical and clinical expertise and often engages in clinical meetings and elements. Dr Barrow currently serves as an Honorary Lecturer at School of Clinical Medicine,

Witwatersrand University and has numerous achievements during his career, amongst which are the following:
• He was involved as an investigator in several clinical trials and is currently working on three new clinical trials on Crohn’s Disease and Ulcerative Colitis
• Presented at International congresses, as recently as International Association of Gastroenterology in Cape Town, Aug 2019 on: “Evaluation of Pancreatic Cystic lesions. What is state of the art?”


Struggling to find work in a healthcare practice?
UCCESSFULLY COMPLETING
AN accredited medical degree and community service is a remarkable achievement. The next step, however, can feel uncertain. Many young healthcare practitioners face a saturated job market, with limited positions available after community service, particularly in specialised fields. For this reason, establishing a private practice has become an attractive and sustainable option. While private practice may seem daunting, it is a realistic and rewarding career path — provided you have the correct support, systems, and knowledge in place.
The South African reality
• Jobs are not always guaranteed after community service
• Communities need more healthcare professionals
• Private practice often feels like a major leap, but it is both possible and viable
• With the right setup, guidance, financing and tools, opening your own consulting rooms is more achievable than it seems.
Common concerns among young doctors
Newly qualified doctors frequently share similar worries about private practice.
• Will I drown in admin instead of treating patients?
Administrative tasks are automated with practice management software, ensuring you can focus on patient care.
• How do I keep patient data safe? GoodX Software is fully POPIA-compliant, ensuring the protection of sensitive information.
• What if I choose the wrong billing or setup?
Built-in, tried-and-tested workflows for the South African healthcare sector guide you through best practices.
• What if I don’t know where to start?
The How to Start Your Practice GoodX online short course provides a step-bystep framework, from setup to daily operations.
THE ESSENTIALS FOR ESTABLISHING
A PRIVATE PRACTICE
Every successful practice in South Africa is
built on a few key foundations:
1. Practice management software – your cornerstone for smooth administration.
2. Reliable hardware – computer, printer, and internet backup.
3. Premises and medical equipment – a suitable space and tools for consultations.
4. Registrations and compliance –HPCSA, BHF, and other registrations are essential.
5. Administrative support –whether through staff or software, efficiency matters.
Why GoodX Software makes it possible GoodX has been developed with South African doctors in mind, ensuring it is relevant to the local market. It provides:
• Time efficiency – spend less time on billing and paperwork, more on patients
• POPIA compliance – data is secure, protected, and accessible
• Local integration – seamless connections with South African medical schemes and healthcare systems
• Scalability – begin as a solo practitioner
and expand as your practice grows
• Accessible design – clear, easy-to-use features with straightforward terminology
• Dedicated support – more than just software; a partner in your professional journey.
CONCLUSION
Becoming a doctor is the most difficult part of the journey. Opening your own practice is the next natural step — one that offers independence, growth, and long-term security.
With GoodX Software and the How to Start Your Practice GoodX online short course, you gain not only the tools but also the confidence to establish a successful private practice in South Africa to serve your community better.
Start your practice today — with GoodX Software, the future of your practice begins now.
For more information, visit goodx.co.za and courses.goodx.co.za.







Focusing the spotlight on antimicrobial resistance
THE SUMMIT BROUGHT to focus, one of the biggest healthcare challenges we face today-AMR. The event underscored the urgent need for improved infection prevention, antimicrobial stewardship, and evidence-based approaches to enhance patient outcomes in wound care.
OVERVIEW
The summit opened with a welcome address from Ross Moore, Commercial Director for South Africa and Anglophone Africa at Essity, who highlighted the organization’s commitment to advancing clinical excellence through innovation. He encouraged delegates to engage deeply with the challenges of infection control within their respective clinical settings.
Speakers across multiple disciplines addressed critical components of Infection Prevention and Control (IPC) and Antimicrobial Resistance (AMR) in wound management. Discussions emphasized the global and local implications of AMR and the shared responsibility among clinicians to mitigate its progression through
stewardship, innovation, and patientcentered care.
URGENCY OF ANTIMICROBIAL STEWARDSHIP
Professor George Smith (Hull York Medical School) emphasized the growing global crisis of AMR, noting that the problem is not a distant threat but a present clinical reality. He stressed the need for multidisciplinary collaboration and sustained global commitment to reversing resistance trends.
Local speaker Dr Febe Bruwer echoed these sentiments, warning against the indiscriminate use of high-potency antimicrobial agents. She cautioned that inappropriate prescribing practices may result in short-term gains but long-term therapeutic losses, advocating instead for accurate diagnosis, appropriate dosage selection, and ongoing treatment evaluation.
Complementing these insights, Dr Nicki Allorto, a leading burn care expert, emphasized the need to strengthen diagnostic and infection management skills not only for wound sites but also for

systemic infections, including in palliative care contexts.
THE ROLE OF PATIENT EDUCATION
Sr Zhavandre van der Merwe highlighted the necessity of enhancing patient education as a cornerstone of effective infection control. She stressed the importance of developing patient-specific, simplified, and visually driven educational tools to improve comprehension and adherence to care plans.
INNOVATIONS IN WOUND MANAGEMENT
The summit also showcased Essity’s DACC™-coated dressing technology, Sorbact®, which offers an evidence-based, non-pharmacological approach to infection management. Dr Johanna Husmark, Global Principal Scientist at Essity, presented data demonstrating Sorbact®’s efficacy against a wide range of wound pathogens, including resistant strains, without contributing to antimicrobial resistance. Adding a strategic perspective, Louise Canonico, Global Marketing Manager for Infection Management at Essity, noted that the rising

prevalence of AMR necessitates “smarter and more responsible wound management strategies” to safeguard patient outcomes and preserve treatment efficacy.
CONCLUSION
The Essity Wound Infection Summit 2025 reaffirmed the organisation’s leadership in advancing wound infection management through scientific collaboration, clinical evidence, and innovative solutions.
Kavitha Ramkhelawan, Essity’s Head of Marketing, closed the event by emphasising that the summit marked the beginning of broader collaborations and continued engagement among all participants. She highlighted the shared commitment to increasing awareness of antimicrobial resistance (AMR), revolutionising the management of wound infections, improving patient outcomes, and reducing associated healthcare costs. Overall, the event’s interdisciplinary discussions provided valuable insights for clinicians, researchers, and policymakers striving to combat AMR and promote sustainable, evidence-based wound care practices.

D I C TA B L E,
R O V EN & PAT I E N T PR E F ERRED 1-1 2 * † ‡§¶

T O H E L P A C HI E V E Y O UR
PAT I E N T S ’ G O A L S
*More peer-reviewed publications (clinical and non-clinical studies) than any other botulinum toxin; therapeutic and aesthetic use; data as of July 31 2022.9 †More clinical studies than any other botulinum toxin; therapeutic and aesthetic use; data as of 24 August 2022.10 ‡Safety profile and efficacy established in clinical trials with more than 23,500 patients treated with BOTOX®; therapeutic and aesthetic use; data as of 31 December 2021.11 §Vs Dysport®; open-label, crossover study to evaluate whether switching botulinum toxin type A formulations affects patient satisfaction (N=40). Patients who were satisfied or extremely satisfied with BOTOX® treatment for CFL+FHL+GL in the preceding 6 months were treated with Dysport® (replicated at a 1:2.5 dose ratio) once the effects of BOTOX® started to diminish. Preference was evaluated at study endpoint at 16 weeks (20 weeks for BOTOX®). A significantly higher proportion of patients preferred BOTOX® (69%) over Dysport® (31%) at the study endpoint (p≤0.05).12 ¶Vs Incobotulinumtoxin-A; retrospective, real-world chart review in Argentinian women (N=110) who had 2 glabellar line treatment cycles with BOTOX® (Period 1) followed by treatment with Incobotulinumtoxin-A (Period 2), with the option to either switch back to BOTOX® (Period 3) or stay with Incobotulinumtoxin-A. Treatment switching was a secondary endpoint: 84% of patients switched back to BOTOX®; 16% stayed on Incobotulinumtoxin-A. Total dose used was not significantly different for BOTOX® and Incobotulinumtoxin-A during Periods 1–3, with a mean glabellar line dose of 15.2 U and 15.3 U per treatment cycle, respectively (primary endpoint).13

REFERENCES: 1. BOTOX® Professional Information, August 2024. 2. Beer KR et al. J Drugs Dermatol. 2011;10(1):39–44. 3. Carruthers JA, et al. J Clin Res. 2004;7:1–20. 4. Glogau R, et al. Dermatol Surg. 2012;38(11):1794–803. 5. Carruthers A, et al. Dermatol Surg. 2014;40(11) 1181–90. 6. De Boulle K, et al. Dermatol Surg. 2018;44(11):1437–48. 7 Trindade de Almeida AR, et al. Dermatol Surg. 2015;41(Suppl 1):S19–S28. 8. Fagien S, et al. Dermatol Surg 2017;43(Suppl 3):S274–S284. 9. Data on file. Allergan Aesthetics. BOTOX® number of peer-reviewed ar ticles vs competitors. August 2022. 10. Data on file. Allergan Aesthetics. BOTOX® number of clinical trials vs competitors. August 2022. 11. Data on file. Allergan Aesthetics. BOTOX® number of patients treated in clinical trials. August 2022. 12. De Boulle KD, et al. J Cosmet Laser Ther. 2008;10(2):87–92. 13. Banegas RA, et al. Aesthet Surg J 2013;33(7):1039–45. BOTOX® Vacuum-dried injection. Contains botulinum toxin type A 50, 100 or 200 units per vial. Registration number: South Africa: 27/30.4/0164. Botulinum toxin units are not interchangeable from one product to another. Doses recommended in Allergan units are different from other botulinum toxin preparations. For full prescribing information refer to the professional information approved by the medicines regulatory authority, accessible by e-mailing medicalinfo.za@abbvie.com. AbbVie (Pty) Ltd, Reg. 2012/068113/07. Address: Building 7, Waterfall Corporate Campus, 74 Waterfall Drive, Midrand, 1685, South Africa. Tel: 011 031 1600. For adverse events, report to MEAPV@abbvie.com. Date of Publication of this material: August 2025. Promo. No. ZA-BCT-250008
The predictable path: evidence-based botox in aesthetic medicine
The advent of onabotulinumtoxinA has transformed aesthetic medicine, establishing it as the gold standard in facial rejuvenation over two decades.
This is a summary of a CPD-accredited article available on www.medicalchronicle.co.za

EYOND EFFICACY, ITS unparalleled predictability builds patient confidence and transforms clinical practice. Backed by robust scientific evidence, patient-reported outcomes (PROs), and comprehensive safety data, onabotulinumtoxinA has created a treatment paradigm extending beyond traditional aesthetic scope.
THE FOUNDATION OF PREDICTABILITY
Predictability is crucial in aesthetic medicine for ensuring positive patient outcomes and physician confidence. OnabotulinumtoxinA demonstrates exceptional consistency across diverse patient profiles, treatment cycles, and clinical uses due to its wellunderstood mechanism of action, doseresponse data, and extensive clinical database spanning over 20 years.
Clinical trials involved over 5 800 participants, highlighting consistent efficacy across demographic profiles and facial anatomies.¹ Standardised techniques and validated assessment tools enable predictable outcomes. Long-term studies (up to 26 years) showed no treatment failure or reduction in therapeutic effectiveness across 1 098 treatment cycles, with stable dosing requirements reflecting natural ageing processes rather than resistance.²
This predictable nature allows practitioners to confidently counsel patients about outcomes, fostering trust and adherence to maintenance regimens.
INDICATIONS AND CLINICAL VERSATILITY
OnabotulinumtoxinA holds regulatory approval for treating glabellar lines, lateral canthal lines, and forehead lines, culminating from rigorous randomised controlled trials proving efficacy and safety.¹ Approvals began in Canada (2001), followed by the US (2002), Europe (2003), and China.³ These three facial indications provide comprehensive rejuvenation for the upper-third facial region, addressing dynamic (movement-related) and static lines (visible at rest).¹ Effects last three-six months, depending on patientspecific factors.¹
Beyond regulatory indications, research has expanded to explore applications in lower facial rejuvenation, neck contouring, and emerging uses for skin quality enhancement.¹ These applications underscore onabotulinumtoxinA’s versatility

and suggest untapped therapeutic potential for future indications.
THE PATIENT VOICE: REDEFINING SUCCESS IN AESTHETIC MEDICINE
The shift from clinician-driven assessments to patient-reported outcomes (PROs) has revolutionised success concepts in aesthetic medicine. Validated instruments like the Facial Line Outcomes Questionnaire (FLO-11) and Facial Line Satisfaction Questionnaire (FLSQ) capture dimensions beyond wrinkle reduction, including psychological and emotional benefits.³
Key findings include enhancements in patients’ confidence, self-esteem, and attractiveness, while diminishing negative perceptions like tiredness or anger associated with facial lines³. PROs influence clinical and regulatory processes, with the U.S. FDA, EMA, and others emphasising patient-focused treatment benefits.³
Long-term data reflects high patient satisfaction; 94% of patients reported looking at least two years younger, and 76% perceived themselves as five-12 years younger after 15+ years of treatment.² PRO tools help align treatments with individual patient goals, enabling a tailored, patientcentred approach.³
LONG-TERM SAFETY: THE REASSURANCE OF EXPERIENCE
OnabotulinumtoxinA’s safety profile is well-
documented and reassuring, supported by extensive long-term data. In a 15-year average study spanning 1 098 treatment cycles, adverse events occurred in only 2.18% of treatments, with mild, transient side effects predominating (eg, temporary muscle weakness in a specific facial muscle).² Eyelid ptosis, the most clinically significant adverse event, occurs in approximately 1% of cases, aligning with meta-analyses.¹ Neutralising antibodies, which could reduce efficacy, appeared in only 0.5% of cases across 5 800 study participants.¹
Critically, no evidence of treatment failure or declining efficacy has been found, even with repeat treatments over decades.² Studies analysing long-term anatomical effects noted no permanent alterations in muscle function, facial expression, or tissue structure despite repeated use, underscoring onabotulinumtoxinA’s safety in aesthetic maintenance.²
SCIENTIFIC INNOVATION AND CLINICAL EXCELLENCE
Botulinum toxin has evolved from experimental therapy to a precise, evidencebased medical discipline driven by innovation in clinical practices and patient assessment tools. Patient-reported outcomes tools like FLO-11 and FLSQ, validated across demographics and languages, provide systematic insights into treatment
satisfaction and expectations.³ Evidencebased protocols in injection techniques, dosing algorithms, and combination treatments have refined outcomes and safety through personalisation based on anatomy and patient goals.¹
This structured approach aligns with broader trends in personalised medicine and contributes to more meaningful patientpractitioner relationships.
FUTURE PERSPECTIVES AND EMERGING OPPORTUNITIES
The field of aesthetic botulinum toxin therapy continues to expand. Development of new formulations with varied onset times, durations, and diffusion characteristics may offer additional therapeutic benefits.¹ Combination therapies integrating onabotulinumtoxinA with fillers, energybased devices, or skincare regimens could enhance outcomes further.
Ongoing focus on PROs will deepen understanding of treatment benefits, paving the way for refined goals centred on patient preferences and satisfaction.³
CONCLUSION
The evidence-based progression of onabotulinumtoxinA underscores the power of integrating scientific rigour, comprehensive safety data, and patientfocused care in modern aesthetic medicine. Over two decades, its predictable outcomes have empowered physicians and inspired confidence among patients, ensuring alignment of clinical success with patient satisfaction.³ Key principles of patientcentred care, evidence-based practice, and clinical predictability, will guide future innovations, with onabotulinumtoxinA exemplifying the transformative potential of science in aesthetic medicine.
REFERENCES
1. Brin MF, Maltman J, Chapman MA, Sangha S. Versatility of OnabotulinumtoxinA in Aesthetic Medicine. Dermatologic Surgery. 2024;50(Suppl 9S):S12-S17. doi:10.1097/DSS.0000000000004348.
2: Trindade de Almeida AR, da Costa Marques ERM, Arsie Contin L, Trindade de Almeida C, Miot HA. Long-term consecutive onabotulinumtoxinA injections for facial aesthetic treatment: A real-world study. Dermatologic Surgery. 2025;00(00):1–6. https://doi. org/10.1097/DSS.0000000000004719.
3: Dayan S, Rivkin AZ, Ogilvie P, Carruthers JDA, Wu Y, Lee E, Patel V, Musumeci M. Revealing the patient perspective: Evolution of patient-reported outcome measures in botulinum toxin studies in aesthetic medicine. Journal of Cosmetic Dermatology. 2025;24(7):e70311. https://doi.org/10.1111/ jocd.70311
Invasive meningococcal disease in SA
The devastating reality of invasive meningococcal disease.
Take the quiz for this CPD-accredited article at:

NVASIVE MENINGOCOCCAL DISEASE (IMD) represents a devastating illness² that demands immediate recognition and urgent intervention. The disease is characterised by its rapid onset and progression, capable of leading to death within hours,¹ transforming apparently healthy individuals into critically ill patients in a matter of moments. Even with access to optimal medical care and appropriate antimicrobial therapy, the case fatality rate remains alarmingly high at approximately 17 %.1,2 The disease’s capacity to cause death despite modern medical advances emphasises the paramount importance of prevention through vaccination.1,2
Meningococcal disease manifests as two primary clinical syndromes: meningococcal meningitis, which involves infection of the lining of the brain and spinal cord, and meningococcal septicaemia, characterised by infection of the bloodstream.¹ The disease begins with flulike symptoms that rapidly worsen,¹ making early recognition challenging yet crucial for patient outcomes. Meningococcal disease is a category 1 notifiable medical condition (NMC).1
COMPREHENSIVE CLINICAL PRESENTATION AND DISEASE PROGRESSION
The clinical manifestations of IMD
demonstrate significant variation according to patient age, but all presentations share the common characteristic of rapid progression. In children and adults, symptoms escalate quickly from flu-like symptoms to severe conditions including high fever, seizures, photophobia, purpuric rash, and coma.¹
Specific symptoms in this population include sudden onset of high fever, severe headache, neck stiffness, dislike of bright lights (photophobia), vomiting and severe diarrhoea or stomach pains, painful joints, pale and blotchy skin, very cold hands and feet, seizures, and drowsiness that can deteriorate into a coma.¹
In infants, the presentation may be even more subtle and challenging to recognise, requiring heightened clinical suspicion from healthcare providers. Symptoms can include a high-pitched moaning cry, inactivity, poor feeding, opisthotonus (neck and back arching) and pale and blotchy complexion.¹ These non-specific signs require heightened clinical suspicion, particularly given that infants represent the age group with the highest incidence of disease.²
The late-stage purpuric rash, which does not fade under pressure using the tumbler test, represents a medical emergency.¹ This characteristic rash can appear anywhere on the body and serves as a critical diagnostic indicator requiring immediate intervention.¹
THE DEVASTATING BURDEN OF LONG-TERM SEQUELAE
Beyond the immediate threat to life, IMD inflicts a devastating burden of long-term complications on survivors. Approximately 17 % of survivors suffer from lifelong complications¹ that profoundly impact their quality of life and place significant demands on healthcare systems and families. These complications include loss of limbs, deafness, nervous system problems, and brain damage.¹ Among all survivors, 20 % develop long-term complications.²
EPIDEMIOLOGICAL LANDSCAPE AND SEROGROUP DISTRIBUTION
Meningococcal disease is endemic to South Africa,¹ occurring year-round but demonstrating significant seasonal variation. The disease peaks between June and October,¹ corresponding to the Southern Hemisphere’s winter and early spring months.
The majority of IMD cases in South Africa are caused by serogroups B and W.¹ Recent surveillance data from 2024 demonstrates the continued dominance of serogroup B, which accounted for 21 out of 56 cases where the serogroup was determined.² This represents more than one-third of all identified cases, highlighting the significant contribution of this serogroup to the overall disease burden.² Serogroups W and Y now fluctuate

between second and third place in terms of prevalence.²
AGE-SPECIFIC DISEASE PATTERNS AND VULNERABLE POPULATIONS
Infants experience the highest incidence of disease, with a secondary peak occurring in the 15-24 year age group.¹ In 2023, infants had the highest IMD incidence at 1.6 cases per 100 000 population, while adolescents and young adults aged 15-24 years experienced an incidence of 0.22 per 100 000 persons.²
The dominance of serogroup B is particularly pronounced in the infant population, which experiences the highest incidence of disease. Since 2019, over half of the disease episodes in infants with known serogroups have been attributed to serogroup B, specifically 46 out of 88 episodes.² This statistic is particularly alarming given that infants are at highest risk for severe disease and poor outcomes. Carriage of Neisseria meningitidis in the oropharynx is common, affecting 5%-10% of the population, with peak carriage rates occurring among young adults.¹ The disease spreads person-to-person via respiratory droplets.² Those with complement deficiencies, anatomic or functional asplenia, and those receiving complement inhibitor therapy are at extremely high risk.4 Most IMD episodes in South Africa are sporadic, with few clusters reported.2
GEOGRAPHIC DISTRIBUTION AND SURVEILLANCE CHALLENGES
Geographic variations in disease incidence are evident across South Africa, with provinces along the coast, particularly the Western Cape, exhibiting higher IMD incidence.² The Western Cape reported an incidence of 0.61 per 100 000 in 2023,² reporting almost as or more than twice the incidence of other provinces over the past few years.² However, the overall seasonal, age-based, and serogroup patterns remain consistent across the country.²
National surveillance for laboratoryconfirmed invasive meningococcal disease has been ongoing since 2003 under the GERMS-SA programme.¹ The relatively low reported incidence levels may reflect inadequate surveillance and reporting mechanisms rather than truly low disease burden.² The true incidence of meningococcal disease occurring in South Africa is likely underestimated due to persons not having specimens taken,2 and case numbers from April through September 2024 are incomplete due to the nonfunctionality of the information technology system.² The overall incidence of IMD in South Africa was 0.18 per 100 000 in 2023, representing an increase since 2021 but remaining well below the peak of 1.4 per 100 000 recorded in 2006.² The disease has primarily consisted of sporadic cases, with limited epidemiological links between patients and no new virulent strains or concerning outbreaks detected in recent years.²
THE UNIQUE CHALLENGES POSED BY SEROGROUP B
Serogroup B presents unique challenges that distinguish it from other meningococcal serogroups. From a microbiological perspective, the serogroup B polysaccharide capsule cross-reacts with human antigens, making it poorly immunogenic.³ The variability in disease incidence and the antigenic profile of Neisseria meningitidis group B across geographical areas5 necessitates careful consideration of local epidemiology when developing vaccination strategies.
DIAGNOSTIC APPROACHES AND LABORATORY CONFIRMATION
Laboratory diagnosis relies on culture, polymerase chain reaction (PCR), and microscopic examination.1 Blood cultures should be collected aseptically and transported to the laboratory within 3-4 hours to optimise recovery.¹
Diagnostic protocols for CSF analysis include comprehensive assessments of protein levels, glucose concentrations, microscopy, Gram staining, culture, and antibiotic susceptibility testing.¹ Rapid bacterial antigen detection tests are discouraged due to reliability concerns.¹ The emphasis on rapid and accurate diagnosis is crucial given the disease’s rapid progression and high mortality rate.
TREATMENT AND CLINICAL
MANAGEMENT
Empiric therapy for suspected bacterial meningitis involves intravenous ceftriaxone or cefotaxime based on agespecific dosages.¹ Once meningococcal meningitis or septicaemia is confirmed, high-dose intravenous benzyl penicillin is recommended for 5-7 days.¹
Respiratory droplet precautions and isolation are advised during admission, with transfer to a general ward after 24 hours of treatment with a drug that will eliminate nasopharyngeal carriage.¹ Patients receiving penicillin alone should also receive chemoprophylaxis to eradicate nasopharyngeal carriage.¹ Emergency treatment is emphasised, even before confirmatory diagnostics such as lumbar puncture or imaging are completed.¹ This approach reflects the critical nature of early intervention in improving patient outcomes.
THE EVOLUTION OF VACCINE AVAILABILITY AND STRATEGIES
South Africa has three registered meningococcal vaccines: a quadrivalent conjugate vaccine targeting serogroups A, C, W, and Y, and two recombinant vaccines targeting serogroup B.1 This limitation was particularly concerning given the emergence of serogroup B as the dominant cause of IMD in the country. Both vaccine types should ideally be used for individuals at high risk due to the circulation of multiple serogroups.¹ Realworld studies demonstrate that serogroup B vaccination significantly reduced disease incidence, with a 75 % reduction observed in vaccine-eligible infants.5 These vaccines utilise multiple antigenic components including recombinant NHBA fusion protein, recombinant NadA protein, recombinant fHbp fusion protein, and outer membrane vesicles containing PorA P1.4 antigen.5
The vaccine contains 50 micrograms each of NHBA fusion protein, NadA protein, and fHbp fusion protein, along with 25 micrograms of outer membrane vesicles from Neisseria meningitidis group B strain NZ98/254.5
These antigens are produced using recombinant DNA technology in Escherichia coli cells and are adsorbed on aluminium hydroxide (0.5mg Al³).5 The vaccine also includes excipients such as sucrose and histidine, with residual kanamycin levels specified as being less than 0.01 micrograms per dose.5 The registration of these serogroup B vaccines in South Africa represents a crucial milestone in the country’s ability to address the dominant cause of IMD. This development provides healthcare professionals with tools to protect against the serogroup responsible for the majority of current cases.
VACCINATION STRATEGIES AND IMPLEMENTATION CHALLENGES
Despite the availability of effective vaccines, meningococcal vaccination is not part of the national immunisation programme in South Africa.¹ Vaccines are available for specific high-risk individuals through the public
sector and can be accessed in the private sector when prescribed by a doctor.¹
The vaccine is intended to produce bactericidal antibodies against the four main antigens: NHBA, NadA, fHbp, and PorA P1.4.5 These antigens play a crucial role in predicting protection against invasive meningococcal disease, although protection levels vary due to differential antigen expression across meningococcal strains.5
DOSING SCHEDULES AND ADMINISTRATION PROTOCOLS
The meningococcal group B vaccine follow specific dosing schedules based on patient age. For infants aged 2-5 months, three 0.5 ml doses are administered at least one month apart or two 0.5 ml doses administered at least two months apart, followed by a booster between 12-15 months of age with an interval of at least six months between the primary series and the booster.5⁵ Older infants and children aged six months to 23 months receive two 0.5 ml doses at least two months apart, with a booster depending on the age group. Children 2 to 10 years, adolescents, and adults receive two 0.5ml doses at least one month apart.5 The vaccine is administered via intramuscular injection, with infants receiving injections in the anterolateral thigh and older age groups in the deltoid muscle.5 The vaccine must not be injected intravenously, subcutaneously, or intradermally, and vaccines must not be mixed in the same syringe.5
VACCINE SAFETY PROFILE AND ADVERSE EVENTS
The safety profile of the meningococcal group B vaccine has been characterised through clinical studies.5 In infants and children under 2 years, common side effects include injection site tenderness, fever, irritability, sleepiness, unusual crying, and diarrhoea.5 Rash is very common in children aged 12-23 months. In adolescents and adults, the most frequently reported adverse events are injection site reactions including severe pain, swelling, and redness, along with malaise, and arthralgia.5
The administration of prophylactic antipyretics such as paracetamol is recommended to manage fever.5
REAL-WORLD EFFECTIVENESS EVIDENCE
Data from the United Kingdom demonstrated a significant 75 % reduction in group B IMD cases among vaccineeligible infants following the introduction of the multi-component vaccine into their National Immunisation Program.5 This three-year observational study revealed disease reduction irrespective of vaccination status or strain’s predicted coverage, providing compelling real-world evidence of the vaccine’s effectiveness.5
The vaccine demonstrates comprehensive immunogenicity, with bactericidal antibody responses being high against the fHbp, NadA and PorA P1.4 antigens across populations including
infants, children, adolescents, and adults, with seropositive rates ranging from 99 % to 100 % across all vaccine antigens.5
POST-EXPOSURE PROPHYLAXIS AND OUTBREAK PREVENTION
Prophylaxis should be given to close contacts, including individuals from the same household, intimate partners, individuals sharing sleeping spaces, or those exposed to secretions.¹
Prophylaxis options include a single dose of oral ciprofloxacin, intramuscular ceftriaxone, or a two-day course of oral rifampicin.¹ Although few clusters are reported, chemoprophylaxis is emphasised for close contacts who have had prolonged close contact with the case in the 7 days preceding the illness.² The limited epidemiological links between patients and absence of new virulent strains or concerning outbreaks in recent years² suggests that current prevention strategies are maintaining control of the disease.
SEASONAL TRENDS AND COVID-19 IMPACT
IMD often increases during the winter to spring months, with an early rise in cases noted during January-May 2024.² However, data after June 2024 may be incomplete due to reporting disruptions caused by the failure of automated systems for reporting laboratory-confirmed public sector episodes.²
FUTURE DIRECTIONS AND PUBLIC HEALTH IMPLICATIONS
The emergence of serogroup B as the dominant cause of IMD in South Africa,² combined with the availability of vaccines,5 creates opportunities for significant disease prevention. The devastating consequences of this preventable disease – including the 17 % mortality1 rate and long-term complications – make prevention through vaccination a primary concern in protecting South African populations. Healthcare professionals must recognise the urgency of addressing IMD, maintaining high clinical suspicion for the disease, and advocating for appropriate prevention strategies. The continued surveillance through the GERMS-SA programme² and ongoing monitoring of serogroup distribution will be essential for informing future prevention strategies and vaccine policies.³
REFERENCES
1. National Institute for Communicable Diseases. Meningococcal disease for health care workers. NICD; 2019.
2. Meiring S, de Gouveia, L, Quan V, et al. Increase in meingococcal disease in South Africa continues into 2024: clinicians urged to be on alert.
3. WHO. Meningitis: immunization, vaccines and biologicals. World Health Organization; 2024. Available from: https://www.who.int/teams/immunizationvaccines-and-biologicals/diseases/meningitis
4. CDC. Meningococcal Vaccination: Recommendations of the Advisory Committee on Immunization Practices, United States, 2020. MMWR Recomm Rep. 2020;69(RR-3):1-116.
5. Bexsero. Package Insert. GlaxoSmithKline South Africa (Pty) Limited; 2023.
Aspen’s Dermatology Range




Topical steroid creams or ointments can be applied with “the fingertip method” 1
The Fingertip unit (FTU ) is a useful measure for calculating the amount of topical preparation to apply to each area.2
• It helps patients understand doses.
• The patient will use enough but not waste treatment.
2 Ways to access a FTU guideline that can assist your patients with the application of topical steroid creams and ointments


The amount of cream and ointment squeezed from a tube from the last skincrease to the tip of the index finger of an adult is called the “Fingertip unit” of cream or ointment.1

The fingertip method: A practical approach to topical corticosteroid dosing
The evidence-based FTU approach eliminates dosing guesswork.
TOPICAL CORTICOSTEROIDS
(TCS) are a mainstay in treating dermatological conditions such as eczema and atopic dermatitis. However, suboptimal dosing practices due to unclear instructions and 'steroid phobia' often result in undertreatment, prolonging disease and compromising outcomes.³ To address these challenges, the fingertip unit (FTU) method was developed as an evidence-based, practical guide for standardising TCS dosing. This concise summary for healthcare professionals outlines key components of the FTU method, its clinical benefits, limitations, and real-world implementation strategies.
BACKGROUND AND DEVELOPMENT
OF THE FTU METHOD
Historically, instructions to 'apply sparingly' or “thinly” created confusion among patients and led to inadequate TCS application.³ To address this, the British Dermatology Working Group introduced the FTU as a standardised measurement system that is quantifiable, adaptable for different patient populations, and educational for reassurance about safe corticosteroid use.³ This method simplifies skin-dosing guidelines, improving patient adherence and outcomes.
Rationale:
• Overcomes undertreatment caused by vague dosing instructions
• Addresses steroid phobia with a measurable, reproducible system
• Provides scalable dosing for varying body sizes, ages, and conditions.
DEFINITION AND MEASUREMENT
An FTU refers to the strip of topical medication squeezed from a tube with a 5mm nozzle, extending from the tip to the distal skin crease of the index finger of an adult.¹,²,³ Each FTU equates to approximately 500 mg of product, sufficient to cover an area equivalent to two adult palm surfaces.
KEY POINTS FOR MEASUREMENT:
1. Nozzle diameter: The FTU metric
assumes a 5mm nozzle; products with varying nozzle sizes may alter FTU output. Clinicians should ensure appropriate education if nozzle diameters are inconsistent.
2. Demonstration: Educate patients by showing the FTU technique using their medication tube. Emphasise the importance of making a continuous line from fingertip to distal interphalangeal crease.
3. Patient empowerment: Encourage use of the non-dominant hand to measure the FTU to minimise inadvertent spreading. Guidelines for body areas
Adult recommendations (per skin region):
• Face and neck: 2.5 FTUs
• Chest and abdomen: 7 FTUs
• Back and buttocks: 7 FTUs
• Each arm and hand: 3-4 FTUs
• Each leg: 6-8 FTUs
• Hands and feet: 1 and 2 FTUs respectively.¹,²,³
Paediatric adjustment
Infants and children require proportionally reduced FTUs, reflecting their smaller body surface areas. For example, a 3-6-month-old infant’s arm and hand may only need 1 FTU. Scaling is critical to avoid over- or under-application while ensuring effectiveness.
APPLICATION GUIDELINES
1. Technique:
– Apply TCS in a thin, even layer.
– Rub gently until absorbed; avoid vigorous rubbing that may irritate the skin.
2. Timing:
– Apply to clean, dry skin.
– Optimal application is after bathing, while skin is slightly moist to enhance absorption.
CLINICAL BENEFITS
The FTU method uniquely addresses both therapeutic and psychological barriers to TCS treatment:
1. Improved treatment outcomes:
• Correct dosing ensures adequate coverage, maximising therapeutic efficacy while minimising treatment failures and prolonged disease durations.³
This is a summary of a CPD-accredited article available on www.medicalchronicle.co.za
• Reduces the need for higher-potency corticosteroids or prolonged treatment courses.
2. Enhanced patient education and adherence:
• Clear dosing instructions empower patients, replacing vague terms with measurable parameters.
• Patients gain confidence knowing they are applying 'the right amount' of medication.
3. Combatting steroid phobia:
• By defining 'appropriate dosing', the FTU method alleviates fear of overuse.
• Evidence-based reassurance builds trust between patients and clinicians, enhancing adherence and outcomes.
ADDRESSING PHOBIA AND MISCONCEPTIONS
Steroid phobia, a prevalent concern stemming from misinformation, limits proper TCS use, worsening undertreatment rates.³
The FTU method helps mitigate these fears by explaining the rarity of side effects when TCS are dosed correctly, the importance of adequate application to achieve therapeutic goals, and how the method is based on clinical evidence to ensure safety.
Maintaining transparency in patient discussions is integral to dispelling stigma. Emphasise the risks of underuse while reinforcing the safety and efficacy of evidence-based dosing.
IMPLEMENTATION
1. Patient education:
• Visual and hands-on demonstrations: Use the patient’s own tube to demonstrate an FTU. Show how much to apply to specific body areas
• Educational materials: Share visual aides, laminated FTU reference charts, or instructional leaflets during consultations.
2. Documentation:
• Record FTU instruction in medical notes to ensure continuity of care
• Indicate whether the patient has been taught, their understanding, and the areas needing reinforcement.
3. Prescriptions with specific FTU guidance:
• Improve clarity by specifying FTUs on

prescriptions (eg 'Apply 2.5 FTUs to the face and neck twice daily').
4. Follow-up:
• Reinforce correct use during follow-ups, addressing potential misconceptions about the method or TCS itself.
SPECIAL POPULATIONS
Paediatric and elderly considerations:
• Provide adjusted FTU guidelines based on child or elderly-specific needs (eg age, skin integrity, and caregiver involvement)
• Assess for dexterity issues or cognitive impairments that may hinder proper application and include caregivers in educational efforts.
Variations in packaging:
• Product packaging differences (eg nozzle width variations, use of pumps) may require alternative measurement strategies
• Educate patients on principles of the FTU system rather than rigid measurements.
Extensive skin involvement:
• Patients requiring treatment over large body surface areas may need modified FTU guidelines, with monitoring for systemic absorption risks.
LIMITATIONS
While the FTU provides a robust starting point for dosing guidance, individualisation is often necessary: 1. Patient-specific adjustments: Disease severity, body size, and affected areas may require clinical judgment beyond standard FTU dosages.
2. Measurement inconsistencies: Varying nozzle diameters or non-tube packaging introduces variability in FTU output. Tailor dosing regimens while emphasising the principles behind FTU measurement.
REFERENCES
1. Allergy Foundation South Africa. 28-eczema atopic dermatitis patient leaflet. Accessed 23 June 2020. https://www.allergyfoundation.co.za
2. Wong ITY, Tsuyuki RT, Cresswell-Melville A, et al. Guidelines for the management of atopic dermatitis (eczema) for pharmacists. Can Pharm J (Ott). 2017;150(5):285-297.
3. Bewley A, on behalf of the Dermatology Working Group. Expert consensus: time for a change in the way we advise our patients to use topical corticosteroids. Br J Dermatol. 2008;158:917-920.

VEMLIDY is indicated for: The treatment of chronic hepatitis B (CHB) in adults and paediatric patients 6 years of age and older weighing at least 25 kg with compensated hepatic disease/function.1 Each film-coated tablet contains 25 mg of tenofovir alafenamide.1
CLINICAL | PAEDIATRICS
R Managing childhood constipation
Childhood constipation represents one of the most common gastrointestinal complaints in paediatric practice, affecting approximately 9.5% of children globally, with some populations experiencing rates as high as 30%.¹
ECENT SWEDISH NATIONAL
data demonstrates a concerning sixfold increase in medically treated constipation from 1.2% in 2006 to 7.9% in 2023, highlighting this condition's growing clinical significance.² Functional constipation typically manifests as infrequent bowel movements (fewer than three per week), hard or pellet-like stools, painful defaecation, and excessive straining.
Children may present with faecal soiling, abdominal pain, or behavioural changes including toilet avoidance. The Rome IV criteria provide standardised diagnostic parameters, emphasising the importance of clinical history over invasive investigations in most cases.³ Peak incidence occurs during the preschool years (ages 2-5), often coinciding with toilet training transitions and dietary changes. Girls demonstrate higher
prevalence rates across all age groups, though the underlying mechanisms for this gender disparity remain unclear.²
EVIDENCE-BASED APPROACH
Current NICE guidelines recommend a multimodal treatment strategy combining dietary modification, behavioural interventions, and pharmacological therapy. Initial management should focus on lifestyle
NEW 20 SACHETS A universal problem, occurring in 0,7 – 28 % of the South African Population. Symptoms of constipation include abdominal pain, a poor appetite and faecal incontinence, all of which interfere with the quality of life of the child and his or her family.2
FOR CHILDREN PURGOPED
For the treatment of chronic constipation in children from 2 years of age.¹
2-11 years1
Constipation in children
Purgoped
S0 Reg. No. 42/11.5/0413. PURGOPED (Powder for oral solution). Each 6,9 g sachet of PURGOPED powder contains:
1. Professional Information: Purgoped (Powder for oral solution). 2. Brown R. A., Wood R. J. Constipation in Children. South African Family Practice 55(4) 350-353 (2013). CIPLA MEDPRO (PTY) LTD. Co. Reg. No. 1995/004182/07. Building 9, Parc du Cap, Mispel Street, Bellville, 7530, RSA. Website: www.cipla.co.za Customer Care: 080 222 6662. [1579850342] An iso-osmotic laxative, a combination of macrogol 3350 (polyethylene glycol) and electrolytes. Macrogol 3350 acts by virtue of its osmotic action in the gastro-intestinal tract which includes a laxative effect.1
factors, including adequate fluid intake and fibre-rich foods such as fruits, vegetables, and whole grains. Importantly, unprocessed bran is contraindicated due to associated bloating and potential micronutrient malabsorption. Laxatives represent firstline pharmacological treatment alongside lifestyle modifications. Osmotic laxatives, particularly polyethylene glycol preparations, demonstrate superior efficacy and tolerability compared to stimulant agents.⁵
Treatment duration often extends beyond symptom resolution, with many children requiring 6-12 months of therapy to achieve sustained remission.
TREATMENT CHALLENGES
Clinical success depends heavily on family education and adherence. Parents require clear guidance regarding treatment expectations, potential side effects, and the importance of maintaining therapy even after symptom improvement. Regular follow-up appointments allow for treatment optimisation and early identification of non-responders. Behavioural strategies enhance therapeutic outcomes. Establishing regular toileting routines, particularly after meals to utilise the gastrocolic reflex, proves beneficial. Positive reinforcement systems can help overcome toilet avoidance behaviours common in affected children.
CLINICAL IMPLICATIONS
Untreated constipation may lead to faecal impaction, encopresis, urinary tract infections, and significant psychological distress. Early intervention prevents these complications and improves long-term outcomes. Red flag symptoms warranting specialist referral include failure to pass meconium within 48 hours of birth, neurological abnormalities, or poor growth velocity.
The rising prevalence of childhood constipation demands heightened clinical awareness and proactive management strategies. Healthcare professionals should maintain low thresholds for initiating treatment whilst emphasising family education and support. With appropriate intervention, most children achieve normal bowel function, though sustained treatment commitment remains essential for optimal outcomes.
REFERENCES
1. Vriesman MH, et al. Management of functional constipation in children and adolescents. Nat Rev Gastroenterol Hepatol. 2020;17(3):178-193.
2. Lindberg G, et al. Epidemiology of childhood constipation: a national study of Swedish children. Acta Paediatr. 2024;113(2):245-252.
3. Hyams JS, et al. Childhood functional gastrointestinal disorders. Gastroenterology. 2016;150(6):1456-1468.
4. NICE Clinical Guideline 99. Constipation in children and young people: diagnosis and management. London: NICE; 2024.
5. Gordon M, et al. Osmotic and stimulant laxatives for the management of childhood constipation. Cochrane Database Syst Rev. 2016;8:CD009118.

Find
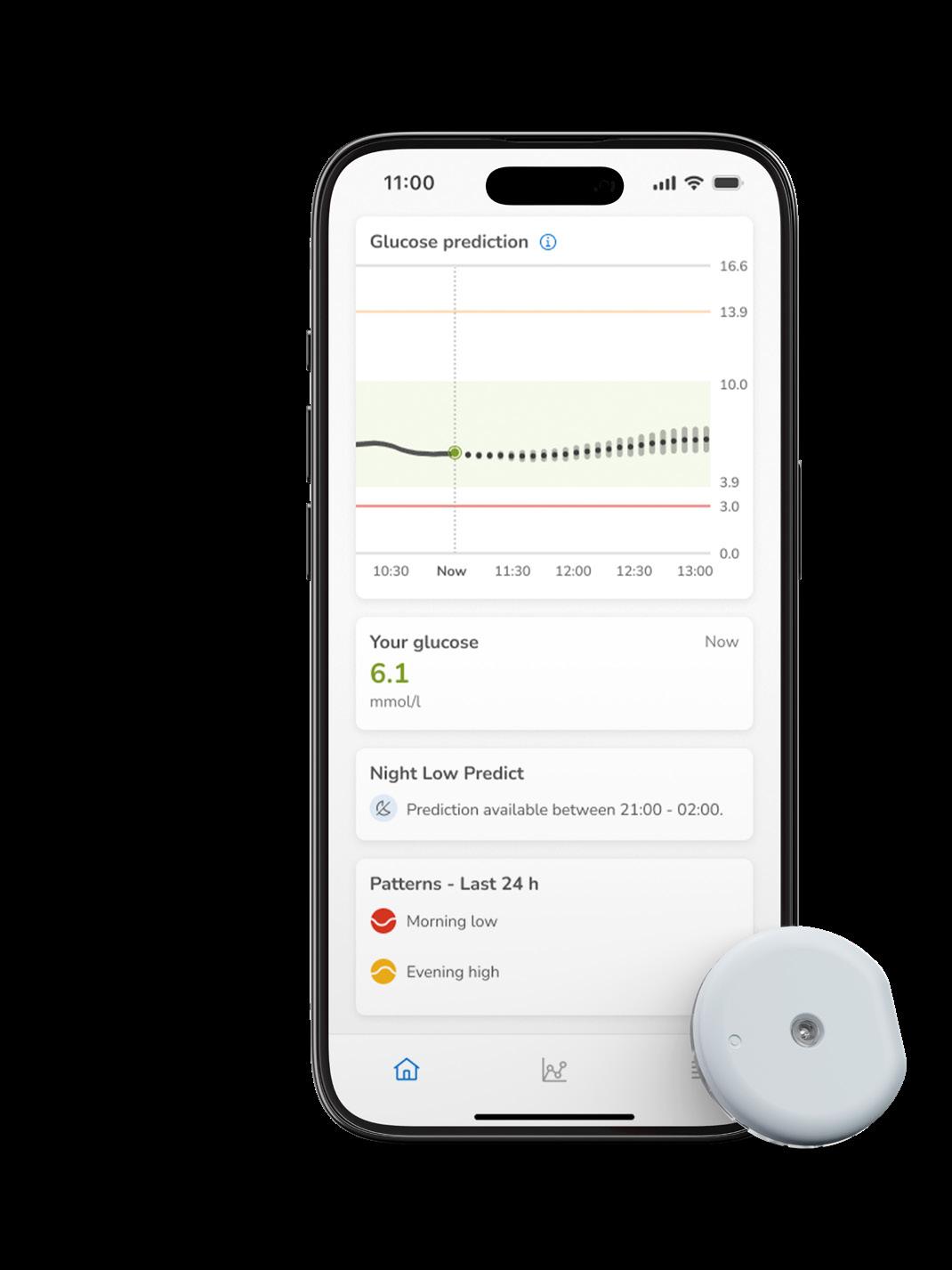


Dr Reyna Daya Physician endocrinologist
Date: 19 November 2025
Time: 19h00
Topic: Monitoring made simple: Transforming diabetes care one click at a time
Speakers: Dr Reyna Daya
Dr Reyna Daya is a specialist physician and endocrinologist working in Gauteng. She is a senior clinician in the Department of Internal Medicine and the Head of the Division of Endocrinology, Diabetes and Metabolism at Helen Joseph Hospital, a tertiary academic hospital attached to the University of the Witwatersrand, Johannesburg, South Africa. Dr Daya is the current chairperson of SEMDSA (Society of Endocrinology, Metabolism and Diabetes of South Africa). She also does limited private practice as a specialist endocrinologist at the Sandton Medi-Clinic. Dr Daya is well known regional and local speaker at


CMEs. She is also an invited editor to multiple National Internal Medicine and Endocrinology Journals. In addition, Dr Daya sits on national drug advisory boards for diabetes and other endocrine disorders. Dr Daya clinical and research interest is in diabetes and thyroid disorders. She is well published in the field of diabetes and endocrinology and holds a masters in medicine from University of the Witwatersrand. Dr Daya is currently working on multiple diabetes related studies as well as supervising Masters students and a number of publications.



































Managing swimmer’s ear: A clinical approach
Otitis externa, commonly known as swimmer’s ear, represents a frequent presentation in South African clinical practice, particularly during the warmer months when water-related activities increase.
THIS INFLAMMATORY CONDITION
of the external auditory canal affects patients across all age groups and requires prompt, targeted intervention to prevent complications and ensure optimal outcomes.
PATHOPHYSIOLOGY AND RISK FACTORS
The external auditory canal’s natural protective mechanisms include acidic pH, cerumen production, and epithelial migration. When these defences are compromised — typically through water exposure, mechanical trauma, or underlying dermatological conditions — the canal becomes susceptible to bacterial and fungal colonisation. Pseudomonas aeruginosa and Staphylococcus aureus represent the predominant bacterial pathogens in acute otitis externa. The warm, humid South African climate, combined with frequent exposure to swimming pools, natural water bodies, and mineral hot springs, creates ideal conditions for microbial proliferation. Patients with diabetes mellitus, immunocompromised states, or chronic skin conditions face elevated risks for severe or recurrent infections.
CLINICAL PRESENTATION
Early recognition of otitis externa relies on characteristic symptomatology. Patients typically present with progressive otalgia, often disproportionate to visible inflammation. The pain characteristically worsens with manipulation of the tragus or pinnan – a key diagnostic indicator distinguishing external from middle ear pathology. Pruritus frequently precedes pain, followed by a sensation of aural fullness. As inflammation progresses, patients may develop purulent discharge, typically yellow-green and malodorous. Hearing loss, when present, results from canal oedema or debris accumulation rather than tympanic membrane involvement.
Physical examination reveals erythema and oedema of the canal walls, often with visible discharge. In severe cases, canal stenosis may prevent adequate visualisation of the tympanic membrane.
EVIDENCE-BASED MANAGEMENT
Effective management requires a dual approach addressing both infection and inflammation. Thorough aural toilet remains the cornerstone of treatment, enabling optimal topical medication penetration whilst removing infected debris.
Topical antimicrobial therapy targeting gram-negative bacteria, particularly Pseudomonas species, forms the primary therapeutic intervention. Fluoroquinolone antibiotics, specifically ciprofloxacin, demonstrate excellent efficacy against the most common pathogens whilst maintaining favourable safety profiles.
The broad-spectrum activity and superior tissue penetration of fluoroquinolones make them particularly suitable for otitis externa management. Concurrent anti-inflammatory treatment proves essential for symptom relief and healing acceleration. Topical corticosteroids, particularly dexamethasone, effectively reduce canal oedema, pain, and inflammatory debris production.
Dexamethasone’s potent anti-inflammatory properties, combined with minimal systemic absorption when applied topically, provide optimal therapeutic benefits whilst minimising adverse effects.
CLINICAL CONSIDERATIONS
South African practitioners should maintain awareness of local resistance patterns
and consider fungal aetiology in chronic or recurrent cases. Patients frequently exposed to natural water sources may require extended treatment courses or prophylactic measures.
References available on request.




CLINICAL | WOMEN'S HEALTH
Menorrhagia: the hidden crisis affecting millions of South Africans
Heavy menstrual bleeding (HMB) represents one of the most underdiagnosed and undertreated conditions affecting South African women, with profound implications for both individual health outcomes and broader public health initiatives.
*Sponsored content
DESPITE AFFECTING 10%-30% of African women according to recent research published in Annals of Medicine & Surgery, this condition remains largely invisible within our healthcare system, perpetuated by cultural stigma, limited awareness amongst both patients and practitioners, and systemic barriers to accessing appropriate care.
THE SCOPE OF THE CRISIS
The magnitude of this health crisis extends far beyond bleeding disorders alone. Research from African Health Sciences demonstrates that over 30% of women with HMB develop anaemia, creating a cascade of health consequences that ripple through every aspect of their lives. These women experience chronic fatigue, cognitive impairment, reduced productivity, and compromised quality of life – yet the underlying cause frequently remains unaddressed.
Vanessa Ascencao, a health and wellness expert specialising in women’s health, describes HMB as a 'hidden health crisis' precisely because of this diagnostic gap. “Many women endure symptoms like fatigue, brain fog, and reduced productivity without seeking help, believing these issues are normal,” she explains. This normalisation of suffering prevents women from receiving timely medical intervention, allowing iron deficiency anaemia to develop and progress unchecked.
CLINICAL RECOGNITION AND RED FLAGS
For frontline healthcare professionals, identifying HMB requires systematic screening beyond traditional gynaecological consultations. Key clinical indicators include:
• Bleeding requiring sanitary product changes every 1–2 hours
• Menstrual periods lasting longer than seven days
• Passage of large blood clots
• Episodes of flooding or breakthrough bleeding
• Associated symptoms of fatigue, dizziness, or cognitive impairment.
However, the diagnostic challenge extends beyond these obvious presentations. Many women present with non-specific symptoms – chronic fatigue, headaches, reduced exercise tolerance, or mood disturbances – without spontaneously connecting these to their
menstrual patterns. This disconnect requires healthcare professionals to actively inquire about menstrual health during routine consultations, particularly when evaluating reproductive-age women with unexplained fatigue or anaemia.
THE IRON DEFICIENCY PARADIGM
The relationship between HMB and iron deficiency represents a critical clinical pathway that demands immediate attention. Unlike other causes of anaemia, HMB creates a chronic, cyclical iron loss that exceeds the body’s ability to compensate through dietary intake alone. Women lose approximately 30-40mg of iron per menstrual cycle under normal circumstances; those with HMB may lose significantly more, creating a negative iron balance that progressively depletes body stores. Ferritin testing should be standard practice in women presenting with HMB, as it provides the most sensitive indicator of iron reserves before overt anaemia develops. Current evidence suggests intervention when ferritin levels drop below 30μg/L, even when haemoglobin remains within normal parameters. This proactive approach can prevent the development of more severe iron deficiency anaemia and its associated complications.
Women should be educated about iron-rich foods and factors that enhance or inhibit iron absorption,enabling themtooptimisetheir nutritional status alongsideprescribed treatments
DIAGNOSTIC CHALLENGES IN CLINICAL PRACTICE
The underdiagnosis of HMB stems from multiple factors within our healthcare system. Cultural taboos surrounding menstruation create barriers to open discussion, whilst limited consultation time may not allow for comprehensive menstrual history-taking. Additionally, many healthcare providers lack specific training in menstrual health assessment, leading to missed
opportunities for early intervention.
To address these challenges, practitioners can implement simple yet effective screening tools. Targeted questions such as “Do your periods ever cause you to miss work or school?” or “Do you feel unusually tired during or after menstruation?” can quickly identify women requiring further evaluation. Point-of-care haemoglobin testing combined with structured menstrual diaries provides objective data to support clinical decision-making.
EVIDENCE-BASED MANAGEMENT STRATEGIES
Effective HMB management requires a multifaceted approach combining medical therapy with supportive interventions. First-line treatments should address both the underlying bleeding disorder and its consequences, particularly iron deficiency. However, the selection of iron supplementation requires careful consideration of patient tolerability and adherence. Traditional iron supplements frequently cause gastrointestinal side effects including constipation, nausea, and abdominal discomfort, leading to poor compliance rates. Newer formulations, such as naturally sourced iron-rich water products like Spatone, offer improved bioavailability with reduced side effects. These gentle alternatives can support iron repletion whilst maintaining patient adherence to treatment regimens.
Lifestyle interventions should complement medical management, including nutritional counselling, stress reduction techniques, and appropriate exercise recommendations. Women should be educated about iron-rich foods and factors that enhance or inhibit iron absorption, enabling them to optimise their nutritional status alongside prescribed treatments.
OVERCOMING BARRIERS TO CARE
Healthcare professionals play a crucial role in dismantling the cultural stigma surrounding menstrual health.
This requires proactive normalisation of menstrual discussions during routine consultations, using non-judgmental language that validates patient experiences. Creating safe spaces for women to discuss their symptoms encourages earlier presentation and more comprehensive history-taking.
Patient education should emphasise when to seek medical attention, specifically:
• Periods requiring hourly sanitary product changes
• Bleeding episodes lasting longer than seven days
• Large clots or flooding episodes
• Fatigue, dizziness, or interference with daily activities.
Women should be empowered to request iron and ferritin testing when experiencing heavy bleeding or unexplained fatigue, ensuring they receive appropriate investigation even when these symptoms are not immediately recognised by their healthcare provider.
IMPLEMENTING SYSTEMATIC CARE PATHWAYS
Private practices can develop comprehensive menstrual health assessment protocols that justify consultation time whilst improving patient outcomes. Structured pathways utilising nursing staff to collect menstrual histories and perform initial blood tests before physician consultations streamline appointments and identify high-risk women efficiently.
A tiered diagnostic approach proves most cost-effective: comprehensive history-taking and basic laboratory tests initially, followed by imaging studies only when uterine pathology is suspected. This strategy balances clinical effectiveness with resource utilisation, ensuring appropriate patient assessment without unnecessary testing.
MOVING FORWARD
Heavy menstrual bleeding represents a significant yet addressable health crisis affecting millions of South African women. By implementing systematic screening protocols, utilising appropriate diagnostic tools, and adopting evidence-based management strategies, healthcare professionals can dramatically improve outcomes for this underserved population. The key lies in recognition – both of the condition itself and of the professional responsibility to actively screen for and address menstrual health concerns. Only through such proactive approaches can we hope to reduce the burden of this hidden crisis and restore quality of life for the countless women currently suffering in silence.









CLINICAL | SMOKING CESSATION
Evidence-based ‘Stoptober’ interventions
As we enter October, the annual Stoptober campaign presents a valuable opportunity to support patients in their smoking cessation journey.
THIS MONTH-LONG initiative, designed to encourage smokers to quit for 28 days, aligns with robust scientific evidence demonstrating that individuals who remain smoke-free for this duration are five times more likely to maintain long-term abstinence.
THE EVIDENCE FOR COMBINATION THERAPY
Recent systematic reviews have strengthened the evidence supporting combination nicotine replacement therapy (NRT) for smoking cessation. Highcertainty evidence demonstrates that combination NRT – typically comprising a nicotine patch alongside a fast-acting form such as gum, lozenge, or spray – results in significantly higher long-term quit rates compared to single-form NRT.¹ The risk ratio of 1.27 (95% CI 1.17 to 1.37) from 16 studies involving 12,169 participants represents a substantial improvement in cessation outcomes.¹ This evidence supports the use of products such as Nicorette combination therapy, where patients benefit from the steady nicotine delivery of patches combined with the flexibility of fast-acting formulations to manage breakthrough cravings. Healthcare professionals should consider recommending combination NRT as a first-line approach, particularly for heavily dependent smokers or those who have experienced difficulty with single-form treatments.
WHO GUIDELINES
The World Health Organization’s Clinical Treatment Guideline for Tobacco Cessation in Adults provides a comprehensive framework for healthcare professionals supporting smoking cessation.² The guidelines emphasise the importance of integrating multiple evidence-based interventions, including behavioural support, pharmacological treatments, and digital tools. Brief advice, lasting 30 seconds to three minutes, should be consistently provided during healthcare encounters.² This simple intervention can significantly impact cessation rates and requires minimal time investment. For patients expressing interest in quitting, more intensive counselling options – including individual face-to-face sessions, group programmes, or telephone support – should be offered.²
PHARMACOLOGICAL INTERVENTIONS
BEYOND NRT
While NRT remains a cornerstone of smoking cessation treatment, healthcare professionals should be aware of the full range of pharmacological options. Varenicline, bupropion, and cytisine are all recommended first-line treatments
for tobacco users interested in quitting.² For individuals experiencing inadequate success with initial treatments, combination pharmacotherapies – such as NRT combined with varenicline or bupropion –represent viable second-line options.²
The duration of NRT use deserves particular attention. While longer durations of treatment (24 weeks versus eight weeks) have not consistently demonstrated significant benefits over shorter durations, the evidence quality for this comparison remains low to moderate.¹ Healthcare professionals should individualise treatment duration based on patient needs and response.
PRELOADING STRATEGIES AND TREATMENT OPTIMISATION
Moderate-certainty evidence supports the use of NRT preloading – initiating treatment before the quit date – as more effective than standard post-quit commencement.¹ This approach may be particularly beneficial during Stoptober, allowing patients to prepare for their quit attempt while managing initial withdrawal symptoms.
Fast-acting NRT formulations demonstrate comparable effectiveness to nicotine patches when used as monotherapy.¹ However, the combination approach consistently outperforms either intervention alone, reinforcing the importance of dual-delivery systems for optimal outcomes.
DIGITAL INTERVENTIONS
Contemporary smoking cessation increasingly incorporates digital technologies. Text messaging, smartphone applications, and artificial intelligencebased interventions serve as valuable adjunctive self-management tools.² These digital platforms can provide continuous support throughout the 28-day Stoptober period, offering personalised advice, progress tracking, and community engagement features.
Healthcare professionals should familiarise themselves with available digital resources and recommend appropriate tools to complement pharmacological and behavioural interventions. The integration of digital support can enhance engagement and provide round-the-clock assistance when traditional healthcare services are unavailable.
SAFETY PROFILE
Systematic reviews consistently demonstrate that serious adverse events are rare across NRT studies.¹ This safety profile supports the use of combination therapy in appropriate patients. Healthcare professionals should counsel patients about

common side effects – such as local skin reactions with patches or jaw discomfort with gum – while reassuring them about the overall safety of NRT interventions.
For patients with cardiovascular concerns, recent evidence supports the safety of NRT in this population, though individual risk assessment remains important. The benefits of smoking cessation far outweigh the minimal risks associated with appropriate NRT use.
IMPLEMENTATION IN CLINICAL PRACTICE
Successful implementation of evidencebased cessation interventions requires systematic approaches within healthcare settings.² Key strategies include:
• Recording tobacco use status in electronic health records as part of routine patient assessments
• Training healthcare providers to deliver evidence-based cessation interventions
• Providing tobacco cessation services at no or reduced cost to eliminate financial barriers
• Establishing clear referral pathways for intensive behavioural support.
Healthcare professionals should receive ongoing training to build skills in delivering evidence-based advice and treatments, supported by prompts, feedback, and quality assurance processes.²
EQUITY AND ACCESSIBILITY
The WHO guidelines emphasise the importance of equity in cessation services.² Healthcare professionals should be particularly attentive to vulnerable populations who may face additional barriers to quitting, including individuals with mental health conditions, lower socioeconomic status, or limited healthcare access.
LOOKING BEYOND OCTOBER
Stoptober campaigns should incorporate strategies to reach diverse communities, ensuring that evidence-based interventions are accessible regardless of demographic characteristics or social circumstances.
While Stoptober provides an excellent catalyst for quit attempts, healthcare professionals should maintain cessation support throughout the year. The 28-day milestone represents the beginning rather than the end of the cessation journey. Longterm success requires ongoing monitoring, relapse prevention strategies, and continued access to support services.
CONCLUSION
Stoptober presents healthcare professionals with an evidence-based opportunity to maximise smoking cessation outcomes. The combination of high-certainty evidence supporting combination NRT, comprehensive WHO guidelines for clinical practice, and innovative digital support tools creates an optimal environment for successful quit attempts.
Healthcare professionals should embrace this annual campaign as a structured approach to implementing best-practice cessation interventions. By combining pharmacological excellence with behavioural support and digital innovation, the healthcare community can significantly impact population health outcomes during October and beyond. The evidence is clear: combination therapy works, brief advice matters, and comprehensive support systems save lives. Stoptober provides the perfect platform to translate this evidence into meaningful patient outcomes.
REFERENCES
1. Theodoulou A, Chepkin SC, Ye W, Fanshawe TR, Bullen C, Hartmann-Boyce J, Livingstone-Banks J, Hajizadeh A, Lindson N. Different doses, durations and modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2023;6:CD013308.
2. World Health Organization. WHO Clinical Treatment Guideline for Tobacco Cessation in Adults. Geneva: World Health Organization; 2023. Licence: CC BY-NC-SA 3.0 IGO.


Chew to activate
Rest between cheek & gum REPEATfor u pto 30 minutes
CLINICAL | WOMEN'S HEALTH
Emergency contraception: A guide
Emergency contraception (EC) represents a critical intervention in reproductive healthcare, offering women the opportunity to prevent unintended pregnancy following unprotected intercourse or contraceptive failure.
ITH OVER 200 MILLION
unintended pregnancies occurring globally each year, healthcare professionals must be well-informed about available options to provide optimal patient care.¹
AVAILABLE METHODS AND MECHANISMS
Emergency contraception encompasses three primary methods: copper intrauterine
devices (IUDs), levonorgestrel (LNG), and ulipristal acetate (UPA). The copper IUD remains most effective with nearly 100% efficacy when inserted within five days.² Among oral options, significant differences exist between LNG and UPA.
Both agents work primarily by inhibiting or delaying ovulation through suppression of the luteinising hormone surge.³ However, levonorgestrel prevents ovulation only when administered before the luteinising hormone
surge begins, limiting its therapeutic window.⁴ In contrast, ulipristal acetate operates as a selective progesterone receptor modulator, maintaining efficacy even when administered closer to ovulation, offering a superior therapeutic advantage.⁵
CLINICAL EFFICACY
The superior efficacy of ulipristal acetate over levonorgestrel has been consistently demonstrated in clinical trials. When

HELPS TO PREVENT PREGNANCY BEFORE IT STARTS!¹
• contains the most effective emergency contraceptive ingredient (ulipristal acetate) when used within the first 24 hours after unprotected sex.²
• the risk of pregnancy is reduced by almost two thirds with compared to levonorgestrel within the first 24 hours.²
is more effective than levonorgestrel in the days leading up to ovulation, because it is the only emergency contraception pill which works even if ovulation is imminent.³

S2 Reg. No. 46/18.8/0280. NS1 Reg. No. 15/18.7/0146. (Namibia) ella®. Each tablet contains 30 mg ulipristal acetate. References: 1. Professional Information: ella® (tablets). 2 Glasier, A. F. et al. Ulipristal acetate versus levonorgestrel for emergency contraception: a randomised non-inferiority trial and meta-analysis. Lancet 375, 555-562 (2010). 3. Brache, V. et al. Ulipristal acetate prevents ovulation more effectively than levonorgestrel: Analysis of pooled data from three randomized trials of emergency contraception regimens. Contraception 88 611–618 (2013). For full prescribing information please refer to the Professional Information approved by the medicines regulatory authority. CIPLA MEDPRO (PTY) LTD. Co. Reg. No. 1995/004182/07. Building 9, Parc du Cap, Mispel Street, Bellville, 7530, RSA. Website: www.cipla.co.za Customer Care: 080 222 6662. [1599562549]
administered within 72 hours, UPA reduces pregnancy risk by nearly 50% compared to LNG.⁶ This advantage becomes even more pronounced in the 72-120 hour window, where UPA maintains significant efficacy while LNG effectiveness wanes considerably. A landmark randomised controlled trial involving 3,445 women revealed pregnancy rates of 1.8% for UPA versus 2.6% for LNG.⁷ Most notably, UPA demonstrated consistent efficacy throughout the five-day window, addressing the critical clinical need as approximately 40% of women seeking emergency contraception present beyond 72 hours.⁸
SAFETY AND TOLERABILITY
Both agents demonstrate excellent safety profiles with similar adverse effects including headache (18%), nausea (12%), and abdominal pain (12%).⁹ Serious adverse events remain exceptionally rare. Neither UPA nor LNG affects established pregnancies or increases miscarriage risk.10 Post-marketing surveillance from millions of users worldwide confirms these favourable safety profiles.
CLINICAL IMPLEMENTATION
Healthcare professionals play a pivotal role in optimising emergency contraception access. Advance provision during routine visits can eliminate time-sensitive barriers.¹¹ Patient counselling should emphasise the time-sensitive nature and superior efficacy of earlier administration.
While the copper IUD offers highest effectiveness, ulipristal acetate represents an excellent oral alternative that bridges convenience and efficacy.¹² Contraindications include hypersensitivity and confirmed pregnancy. Weight may influence effectiveness for both agents, though current guidelines recommend proceeding regardless of BMI.¹³
ADDRESSING ACCESS BARRIERS
Emergency contraception faces numerous access barriers including healthcare system limitations, pharmacy restrictions, and knowledge gaps.¹⁴ Particularly concerning is limited ulipristal acetate availability due to prescription requirements, despite its superior effectiveness.¹⁵
CONCLUSION
Emergency contraception represents a vital tool in preventing unintended pregnancy, with ulipristal acetate offering particular advantages through its extended efficacy window and superior effectiveness compared to levonorgestrel. Healthcare professionals must ensure timely access while understanding the evidence supporting this more effective option to optimise patient outcomes and contribute to broader public health goals.
Multivitamin and amino acid benefits
Nutritional supplementation has become increasingly prevalent in clinical practice, with multivitamins and amino acids representing two of the most commonly recommended interventions.
RECENT SYSTEMATIC REVIEWS
and large-scale clinical trials provide robust evidence supporting the targeted use of these supplements in specific patient populations and clinical contexts. The clinical utility of daily multivitamin supplementation demonstrates population-specific benefits rather than universal health improvements. A large UK Biobank study published in 2024 revealed significant mortality and morbidity reductions in individuals with metabolic dysfunction-associated steatotic liver disease (MASLD), with multivitamin users showing reduced risks of cardiovascular disease, chronic kidney disease, and all-cause mortality.¹ This protective effect likely stems from enhanced antioxidant capacity and reduced systemic inflammation in metabolically compromised patients. Cognitive health represents another area of established benefit. A comprehensive meta-analysis of three large cognition studies demonstrated that daily multivitamin supplementation containing over 20 micronutrients improved memory function and delayed cognitive aging by approximately two years in older adults.² This neuroprotective effect suggests particular clinical relevance for patients at risk of cognitive decline. However, clinicians should note that evidence does not support routine multivitamin supplementation in generally healthy adults. A prospective US cohort study with over 20 years of follow-up found no mortality benefit from daily multivitamin use in healthy populations,³ emphasising the importance of targeted rather than universal supplementation strategies.
AMINO
ACID SUPPLEMENTATION
lising effects through serotonin pathway modulation.⁷ In renal medicine, amino acid supplementation may improve plasma flow and reduce uric acid levels in patients with chronic kidney disease.⁸
CLINICAL RECOMMENDATIONS
Current evidence supports targeted multivitamin supplementation in patients
with metabolic dysfunction, cognitive vulnerability, or documented micronutrient deficiencies rather than routine administration in healthy individuals. EAA supplementation demonstrates broader clinical utility, particularly for muscle health maintenance, exercise recovery, and adjunctive therapy in chronic disease management. Typical dosing protocols
employ 1-1.5g EAAs per 10kg body weight daily, with patient-specific adjustments based on clinical indication and response monitoring.⁹ Consider individual patient factors, existing comorbidities, and potential drug interactions when recommending supplementation protocols.
References available on request.

Essential amino acid (EAA) supplementation demonstrates more consistent benefits across diverse clinical contexts. Recent evidence supports multiple therapeutic applications, particularly in muscle health maintenance and disease management. Muscle function and sarcopenia prevention represent primary indications for EAA supplementation. Clinical trials demonstrate that EAA supplementation effectively maintains muscle mass, improves strength, and supports protein synthesis.⁴ A 2024 study in knee osteoarthritis patients showed significant improvements in gait speed, step count, and quadriceps muscle volume when EAA supplementation accompanied physical therapy.⁵ Exercise recovery and performance enhancement provide additional clinical benefits. Branched-chain amino acids (leucine, isoleucine, and valine) reduce post-exercise muscle soreness, decrease perceived exertion during high-intensity activities, and accelerate recovery compared to placebo interventions.⁶ Emerging evidence suggests broader therapeutic applications. Tryptophan supplementation demonstrates anxiolytic and mood-stabi-



Hyperuricemia and chronic gout:
How to use urate-lowering therapy
Hyperuricemia, defined as serum uric acid (SUA) levels exceeding 6.8mg/dL (0.40mmol/L), affects approximately 20% of adults in developed countries,¹ and represents a significant clinical challenge with far-reaching health implications.
EYOND ITS ROLE as the primary risk factor for gout, emerging evidence highlights hyperuricemia’s association with cardiovascular disease, chronic kidney disease, and metabolic syndrome,² positioning effective urate lowering therapy (ULT) as a cornerstone of comprehensive patient management.
PATHOPHYSIOLOGY AND DISEASE PROGRESSION
Uric acid, the terminal product of purine metabolism, is produced through the sequential action of xanthine oxidase on hypoxanthine and xanthine.³ Under physiological conditions, approximately two-thirds of daily uric acid production is eliminated through renal excretion, with the remainder cleared via intestinal uricolysis.³ Hyperuricemia develops when this delicate balance is disrupted, either through increased purine turnover, enhanced dietary purine intake, or – more commonly –decreased renal uric acid clearance.²
The progression from asymptomatic hyperuricemia to symptomatic gout follows a predictable trajectory. Initial monosodium urate (MSU) crystal deposition in synovial fluid and tissues triggers an inflammatory cascade mediated by the NLRP3 inflammasome, resulting in interleukin-1β release and subsequent neutrophil recruitment.² Without appropriate intervention, acute intermittent gout evolves into chronic tophaceous disease characterised by persistent joint inflammation, structural damage, and reduced quality of life.¹
CLINICAL PRESENTATION AND COMPLICATIONS
Chronic gout presents distinct challenges compared to acute gouty arthritis. Patients may experience persistent low-grade inflammation with ongoing joint pain and stiffness, even between apparent flares.¹ Tophi – pathognomonic nodular deposits of MSU crystals surrounded by inflammatory tissue – develop in approximately 30% of patients with untreated gout within five years of diagnosis.⁴
These subcutaneous and intra-articular deposits commonly affect the first metatarsophalangeal joint, olecranon bursae, and finger joints, potentially causing significant functional impairment and disfigurement.¹ Advanced chronic gout may involve axial skeleton structures, including the sacroiliac joints and spine, presenting diagnostic challenges and increased morbidity.¹
Comorbid conditions significantly influence chronic gout management. Renal impairment, present in up to 60% of gout patients, creates a pathophysiological cycle where hyperuricemia contributes
to nephropathy while reduced glomerular filtration rate impairs uric acid clearance.²
Cardiovascular disease risk increases substantially, with gout patients experiencing 1.5–2.0-fold higher rates of myocardial infarction and stroke compared to unaffected individuals.²
DIAGNOSTIC CONSIDERATIONS
Accurate diagnosis remains fundamental to optimal management. Joint aspiration with polarising light microscopy demonstrating intracellular MSU crystals provides definitive diagnosis, though this is frequently impractical in primary care settings.⁴ The 2015 American College of Rheumatology/ European League Against Rheumatism classification criteria offer enhanced diagnostic accuracy, incorporating clinical features, laboratory parameters, and imaging findings.⁴
Dual-energy computed tomography (DECT) represents a significant advancement in gout diagnosis, enabling non-invasive identification of MSU deposits with 90% sensitivity and 85% specificity.⁴ Ultrasound examination can detect characteristic features including double contour sign and tophi, providing valuable diagnostic and monitoring capabilities in appropriately trained hands.⁴
Contemporary urate lowering therapy
The 2024 European League Against Rheumatism guidelines emphasise early ULT initiation using a treat-to-target approach, aiming to achieve SUA levels below 6.0mg/ dL (0.36mmol/L) for most patients, with more stringent targets of less than 5.0mg/ dL (0.30mmol/L) recommended for patients with tophi or frequent flares.¹,⁴
Allopurinol remains the first-line ULT choice for patients with normal renal function.¹,⁴ This purine analogue inhibits xanthine oxidase competitively, reducing uric acid production while allowing alternative pathway utilisation for purine salvage.⁵ The active metabolite oxypurinol provides sustained enzyme inhibition with an extended half-life of 18–30 hours, enabling once-daily dosing and improved adherence.⁵
Treatment initiation requires careful consideration of the ‘start low, go slow’ principle. Allopurinol should commence at 100mg daily (50mg in patients with chronic kidney disease stage 4 or worse), with dose escalation every 2–4 weeks based on SUA monitoring and tolerability.¹,⁴ Maximum recommended doses range from 300mg daily in severe renal impairment to 900mg daily in patients with normal kidney function, though most patients achieve target SUA levels with 300–600mg daily.¹,⁴
Critical safety considerations include allopurinol hypersensitivity syndrome, a potentially fatal reaction occurring in 0.1–0.4% of patients.⁵ Risk factors include

renal impairment, concurrent diuretic use, and genetic predisposition – particularly the HLA-B*5801 allele prevalent in populations of East Asian descent.1,4 Pre-treatment screening is recommended for high-risk patients, with febuxostat representing an appropriate alternative in allopurinolintolerant individuals.1,4
Flare prophylaxis and monitoring
ULT initiation paradoxically increases gout flare risk during the first 6–12 months of treatment due to MSU crystal dissolution and mobilisation.1,4 Prophylactic therapy using colchicine 0.5mg once or twice daily represents the preferred approach, with non-steroidal anti-inflammatory drugs or low-dose prednisolone (≤10mg daily) serving as alternatives in colchicineintolerant patients.1,4
Contrary to historical practice, ULT should continue during acute flares to prevent treatment interruption and maintain steady-state uric acid suppression.1,4 This approach, supported by robust clinical evidence, prevents the ‘yo-yo’ effect of fluctuating SUA levels that can perpetuate crystal deposition and inflammatory responses.1,4
Regular monitoring encompasses SUA measurement every 2–4 weeks during dose titration, followed by annual assessment once target levels are achieved.1,4 Additional parameters include renal function, liver enzymes, and full blood count, particularly during initial treatment phases.
⁵
Future directions and conclusion Emerging therapeutic strategies include selective uric acid reabsorption transporter 1 (URAT1) inhibitors such as lesinurad, which enhance renal uric acid excretion when combined with xanthine oxidase inhibitors.⁶ Pegloticase, a pegylated uricase
enzyme, offers hope for refractory cases, though immunogenicity concerns limit broader application.
⁶
Optimal chronic gout management requires comprehensive understanding of disease pathophysiology, appropriate diagnostic techniques, and evidence-based ULT implementation. Allopurinol remains the cornerstone of treatment, with early initiation, adequate dosing, and appropriate monitoring facilitating achievement of therapeutic targets and improved long-term outcomes.1,4,5
Healthcare professionals should embrace proactive management strategies, recognising that effective urate lowering therapy not only prevents gout-related complications but may also confer broader cardiovascular and renal benefits for this high-risk patient population.²
REFERENCES
1. Richette P, Doherty M, Pascual E, et al. 2016 updated EULAR evidence-based recommendations for the management of gout. Ann Rheum Dis. 2017;76(1):29-42.
2. Johnson RJ, Bakris GL, Borghi C, et al. Hyperuricemia, acute and chronic kidney disease, hypertension, and cardiovascular disease: report of a scientific workshop. Hypertension. 2018;71(6):e1-e8.
3. Hille R, Nishino T, Bittner F. Molybdenum enzymes in higher organisms. Coord Chem Rev. 2011;255(910):1179-1205.
4. Neogi T, Jansen TL, Dalbeth N, et al. 2015 Gout classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2015;74(10):1789-1798.
5. Day RO, Graham GG, Hicks M, et al. Clinical pharmacokinetics and pharmacodynamics of allopurinol and oxypurinol. Clin Pharmacokinet. 2007;46(8): 623-644.
6. Sundy JS, Baraf HS, Yood RA, et al. Efficacy and tolerability of pegloticase for the treatment of chronic gout in patients refractory to conventional treatment. JAMA. 2011;306(7):711-720.
ALLOPURINOL
100 Cipla
Allopurinol 100 mg
S3
ALLOPURINOL
300 Cipla
Allopurinol 300 mg
INDICATIONS1
ALLOPURINOL CIPLA is indicated for the treatment of gout and hyperuricaemia associated with other conditions.

It may be effective in patients with impaired renal function.
ALLOPURINOL CIPLA is also used in the treatment of hyperuricaemia associated with leukaemia or resulting from radiotherapy or the use of antineoplastic agents such as mercaptopurine, or during treatment with diuretics of the thiazide or similar type.


Broad-spectrum vaginal antiseptics in clinical practice: PVP-I gel formulations for comprehensive mixed
infection management
Modern povidone iodine (PVP-I) gel formulations in vaginal health management represent a sophisticated approach to addressing the complex nature of mixed infections whilst preserving epithelial integrity and supporting beneficial microbiome function.
S ANTIBIOTIC RESISTANCE
continues to escalate globally, current PVP-I gel formulations offer clinicians valuable alternatives that combine established broad-spectrum antimicrobial efficacy in an antiseptic with advanced formulation properties that provide osmolyte-based protection and microbiome-preserving characteristics. Understanding how contemporary PVP-I gel formulations integrate these features has become essential for optimal patient outcomes, particularly given the significant psychological burden associated with recurrent vaginal infections.
CLINICAL BURDEN OF MIXED VAGINAL INFECTIONS AND THE PVP-I GEL ADVANTAGE
Vaginitis represents one of the most prevalent gynaecological presentations, with women experiencing 45% higher depression scores and 70% higher anxiety scores compared to healthy controls, as symptoms including discharge, odour, itching, irritation, and burning contribute to anxiety, shame, and hygiene concerns. The complexity of managing these conditions lies in their polymicrobial nature, requiring comprehensive antimicrobial approaches that current antiseptics like PVP-I gel formulations are uniquely positioned to address. PVP-I gel formulations demonstrate exceptional suitability for mixed infection management through proven broad spectrum activity against bacteria, viruses, fungi, yeasts, moulds, and protozoa. The three primary infectious causes of vaginitis - bacterial vaginosis (40-50% of cases), vulvovaginal candidiasis (20-35% of cases), and trichomoniasis (5-20% of cases) - frequently coexist as polymicrobial infections where PVP-I’s comprehensive antimicrobial coverage provides essential therapeutic advantages over narrow-spectrum treatments.
Contemporary antiseptic PVP-I gel formulations utilise the sustained release properties of the povidone-iodine complex, delivering optimal antimicrobial activity through advanced formulation technologies that address the limitations of traditional antiseptic approaches. The sophisticated formulation science enables antiseptic PVP-I gels to maintain established efficacy whilst incorporating properties that support long-term vaginal health maintenance.
PVP-I GEL FORMULATIONS WITH INTEGRATED EPITHELIAL PROTECTION
Current PVP-I gel formulations incorporate osmolyte-based principles that provide essential epithelial barrier protection during antimicrobial treatment, addressing a critical advancement in vaginal antiseptic therapy. Clinical research demonstrates that healthy vaginal fluid maintains an osmolality of approximately 370 ± 40 mOsm/kg, and modern PVP-I gel formulations are designed to work within these physiological parameters to support rather than compromise tissue integrity.³
Contemporary PVP-I gel formulations maintain osmolality characteristics that preserve epithelial barriers and tissue structure whilst delivering effective antimicrobial activity.³ This formulation approach enables PVP-I gels to provide established broad spectrum efficacy whilst preventing the cytotoxic effects associated with hyperosmolal formulations that exceed 1,500 mOsm/kg and cause epithelial barrier disruption.
The sophisticated formulation of current antiseptic PVP-I gels creates a dualaction approach where the established antimicrobial mechanisms of povidone iodine - including oxidation of amino acids and nucleic acids, metabolic disruption, and cell membrane destabilisation - operate synergistically with formulation-mediated epithelial protection. This combination addresses both immediate pathogen elimination and tissue integrity preservation, essential for preventing the recurrence rates of 50-67% associated with treatments that fail to preserve epithelial barrier function.
MICROBIOME-COMPATIBLE PVP-I GEL DELIVERY
SYSTEMS
Modern antiseptic PVP-I gel formulations represent a significant advancement from traditional antiseptic approaches by incorporating microbiome-compatible delivery systems that support the preservation and restoration of beneficial Lactobacillus populations whilst maintaining comprehensive antimicrobial efficacy against pathogenic organisms. This represents a paradigm shift towards selective pathogen targeting rather than broad microbial elimination.
Lactobacillus species provide essential protection through lactic acid production, maintaining vaginal pH below 4.5, and producing bacteriocins that selectively target pathogenic bacteria whilst preserving beneficial organisms.² The sustained release characteristics of current antiseptic PVP-I gel formulations enable controlled antimicrobial activity that eliminates
pathogens whilst creating conditions favourable for lactobacillus recolonisation following treatment. Contemporary antiseptic PVP-I gel formulations incorporate pH-compatible systems that maintain the acidic environment essential for lactobacillus dominance whilst delivering effective antimicrobial activity against the full spectrum of organisms implicated in mixed infections. This approach leverages PVP-I’s multi-target mechanisms to address biofilm-forming pathogens that resist conventional treatments whilst supporting the competitive exclusion mechanisms employed by beneficial bacteria.²
pH-OPTIMISED PVP-I
GEL FORMULATIONS FOR COMPREHENSIVE INFECTION MANAGEMENT
Current antiseptic PVP-I gel formulations integrate pH optimisation technology with established antimicrobial mechanisms to create therapeutic systems that address both immediate pathogen elimination and underlying pathogenesis factors. These sophisticated formulations maintain PVP-I’s broad spectrum antimicrobial efficacy whilst incorporating pH-modulating properties that support vaginal health restoration.
This advanced formulation approach enables contemporary PVP-I gels to function optimally within physiological pH ranges whilst supporting the restoration of environmental conditions that favour beneficial microorganisms. The pH optimisation enhances PVP-I’s natural antimicrobial mechanisms whilst creating synergistic effects with the body’s natural protective systems, including the acidproducing capabilities of lactobacilli.
Modern PVP-I gel formulations demonstrate superior outcomes in clinical applications through their comprehensive approach that addresses the complex interplay between pathogen elimination and microbiome restoration. This positions current PVP-I gel technology as the optimal antiseptic with antimicrobial properties for therapeutic applications that require both immediate efficacy and long-term vaginal health support.
CLINICAL APPLICATIONS OF CONTEMPORARY PVP-I GEL FORMULATIONS
The clinical implementation of current PVP-I gel formulations provides healthcare professionals with therapeutic options that combine established antiseptics providing antimicrobial efficacy with advanced
formulation technologies addressing the complete spectrum of vaginal health needs. These formulations leverage PVP-I’s proven track record against resistant pathogens whilst incorporating properties that support epithelial integrity and microbiome balance.
Contemporary PVP-I gel formulations prove particularly valuable for patients with recurrent infections where traditional treatments have failed to provide sustained relief. The combination of broad spectrum antimicrobial activity with integrated tissue protection and microbiome compatibility addresses the multifactorial nature of recurrent presentations whilst minimising the tissue damage and microbiome disruption associated with repeated antimicrobial treatments.
Clinical evidence supports approaches where current PVP-I gel formulations work synergistically with the body’s natural protective mechanisms, particularly supporting Lactobacillus crispatus populations, to reduce recurrence rates whilst providing immediate symptom relief.² This integrated approach demonstrates superior outcomes compared to antimicrobial-only treatments by addressing both pathogen elimination and beneficial bacteria preservation through sophisticated formulation design.
ADVANCED FORMULATION SCIENCE IN CURRENT PVP-I GEL TECHNOLOGY
Contemporary antiseptic PVP-I gel formulations represent sophisticated integration of osmolyte principles, pH optimisation, and sustained release mechanisms whilst maintaining the antimicrobial potency that makes PVP-I uniquely effective for mixed infections. Current formulation science has enabled the creation of PVP-I gels that deliver consistent antimicrobial activity whilst incorporating protective and restorative features that represent significant advancement over traditional antiseptic approaches.
The sustained release properties of the povidone-iodine complex in current gel formulations provide an ideal platform that maintains epithelial barrier integrity throughout the treatment period. This controlled delivery approach ensures that PVP-I’s broad spectrum antimicrobial mechanisms operate within an environment optimised for tissue protection and beneficial bacteria preservation.
References available on request

VAGINITIS
VAGINITIS:
VAGINITIS:
THE MOST COMMON GYNAEGOLOGICAL PROBLEM IN PRIMARY CARE15
CHARACTERISED BY15:
•Concerns
THE MOST COMMON GYNAEGOLOGICAL PROBLEM IN PRIMARY CARE15
The most common gynaecological problem in primary care.1 Yet, adequate diagnosis and treatment of vaginitis is often problematic.2
VAGINITIS: THE MOST COMMON GYNAEGOLOGICAL PROBLEM IN PRIMARY CARE15
VAGINITIS: THE MOST COMMON GYNAEGOLOGICAL PROBLEM IN PRIMARY CARE15
CHARACTERISED BY15:
CHARACTERISED BY15:
CHARACTERISED BY15:
Characterised by:1 BETADINE® PVP-I has a broad antimicrobial spectrum3,4
Discharge Odour Itching Irritation IMPACTS QUALITY
IMPACTS QUALITY OF LIFE NEGATIVELY15:
•Anxiety
•Shame
IMPACTS QUALITY OF LIFE NEGATIVELY15: •Anxiety •Shame
CHARACTERISED BY15: VAGINITIS ACCOUNTS
•Concerns
•Concerns about hygiene, especially with recurrent symptoms
THE THREE MOST COMMON INFECTIONS
THE THREE MOST COMMON INFECTIONS19
THREE MOST COMMON INFECTIONS
TRICHOMONIASIS: 5%-20% OF CASES
TRICHOMONIASIS: 5%-20% OF CASES
VULVOVAGINAL CANDIDIASIS: 20%-35% OF CASES
VULVOVAGINAL CANDIDIASIS: 20%-35% OF CASES

VULVOVAGINAL CANDIDIASIS: 20%-35% OF CASES

40%-50% OF
VAGINITIS ACCOUNTS FOR 10% OF ALL DOCTOR VISITS


HEALTHCARE16 AND ARE 6 TIMES MORE COMMON URINARY TRACT INFECTIONS
VAGINITIS ACCOUNTS FOR 10% OF ALL DOCTOR VISITS FOR

The overlooked health crisis hiding in your mouth

South Africa is lagging behind because we refuse to confront the obvious: patients are not educated about the social determinants of health, and the commercial determinants of health that are destroying lives are systematically ignored. Our policies are written in policy-speak that communities cannot understand. That failure shows up in the dental chair, in our hospitals, and in the statistics of preventable diseases.
TO ESTIMATE SMOKING prevalence and frequency among both adolescents (10-17 years) and adults (>18 years) Take sugar. If we were serious, sugary products would not sit in aisles at children’s eye level. They would not be pushed as daily staples. They would be treated as the harmful substances they are. Instead, big businesses use their powers and advocate for their profits and ensure that their brands remain untouchable. Profit wins, health loses. Communities reach for sugar because it is cheap, accessible, and comforting, and in return, they get rotting teeth and are prone to the prediabetes stage and other chronic diseases.
Anything sweet tends to be soothing, but that comfort comes at a price. A mouth constantly bathed in sugar is at high risk of developing dental caries. Sugary beverages do not just erode teeth, they push people toward prediabetes and obesity. Once too much sugar enters the body, tooth decay is inevitable, and chewing becomes painful. Nutrition suffers, well-being declines, and people are left with poor quality of life. The damage begins in childhood and
compounds with age, ensuring that preventable diseases are attended to and it is a life course approach.
This is not just about toothache and periodontal diseases; we need to ensure that oral diseases are addressed earlier on in life. Harm reduction is about survival and an alternative to harmful behaviour. It is also about preventing other conditions such as squamous cell carcinoma in smokers and heavy drinkers. These diseases may have negative impact on the users’ quality of life. Harmful reduction is also about minimising trauma-related oral injuries. It is about offering alternatives such as e-cigarettes or nicotine pouches instead of cigarettes, safer diets instead of sugar overload. Harm reduction is not indulgence. It is survival.
Patients themselves report that switching to alternatives helps with their cravings. Many say e-cigarettes and heated tobacco products reduce their craving for cigarettes. Research must continue, but the principle is clear that harm reduction improves health outcomes. Yet patients must not be judged for making these choices. Harm reduction is not about
replacing one habit with another, but about lowering the risks that destroy health. If people are left without options, they are condemned to continue patterns of consumption that guarantee disease.
Passive smoking continues to harm children every day because parents are not taught the truth. Carcinomas do not arrive suddenly, but there can be predictable poor health outcomes if diseases are not attended to. Policy makers need to protect people over profits. Periodontal disease also has this bidirectional relationship with diabetes, smoking tobacco becomes a compounding factor to this. The silence is not ignorance and it is well-calculated by those who benefit from sales.
Oral health is not cosmetic and it must be seen as the frontline of public health. By the time patients reach a dentist for extractions, root canals, or bridges, the damage is already catastrophic. They cannot chew, cannot eat properly, and their dignity is eroded. Secondary and tertiary prevention should be the norm. Primary prevention is about brushing twice a day with fluoridated toothpaste, flossing, scaling and polishing,
and it is not a luxury. It is the foundation of oral health. When access to these basics is limited by poverty, policy must step in.
Prevention demands courage and it means saying no to unhealthy foods and beverages. It means enforcing correct and visible labelling for brands. It means pushing sugar out of reach. It means educating children, parents, and communities with information they can use, not jargon that gathers dust in a policy binder. It means telling the truth even when it offends those who profit. Harm reduction is not optional. It is the only way forward. To continue ignoring it is reckless and unethical.
South Africa must decide: do we continue to allow poor health outcomes and weak policies to direct our health? Or do we lead with courage, honesty and action?
Oral hygiene is key to harm reduction. Oral hygiene is key to health. Oral hygiene is key to life. Anything less is negligence. Dr Pumela Gwengu, HOD of the Department of Operative Dentistry at the Sefako Makgatho Health Sciences University & Specialist in community dentistry.
Dual-action therapy in infectious keratitis
Balancing anti-inflammatory and antimicrobial strategies.
THE MANAGEMENT OF infectious keratitis presents a complex clinical challenge, particularly when significant inflammation accompanies bacterial infection. The decision to combine topical corticosteroids with antimicrobial therapy requires careful consideration of timing, patient selection, and potential risks.
COMBINATION THERAPY
The landmark Steroid for Corneal Ulcers Trial (SCUT), a randomised controlled trial involving 500 patients, provided crucial evidence regarding adjunctive corticosteroid use in bacterial keratitis.¹ The study demonstrated no overall difference in three-month visual acuity between patients receiving combination steroid-antibiotic therapy versus antibiotics alone, importantly showing no increase in adverse events such as corneal perforation or need for surgery.¹
However, subgroup analyses revealed nuanced benefits, suggesting potential advantages of steroids in severe ulcers, non-Nocardia infections, and selected Pseudomonas cases, particularly when initiated after 48 hours of effective antibiotic treatment.² These findings highlight the importance of individualised treatment decisions rather than blanket protocols. The inflammatory response in infectious keratitis involves both beneficial antimicrobial effects and potentially harmful tissue damage. While inflammation helps eliminate pathogens, excessive inflammatory responses can lead to corneal scarring, thinning, and neovascularisation.³ Topical corticosteroids can mitigate these harmful effects by reducing inflammatory cell infiltration and cytokine production while preserving visual outcomes. In South Africa, bacterial conjunctivitis and keratitis present unique epidemiological challenges. Poor sanitation and limited access to clean water in some communities contribute to higher infection rates. Additionally, the high prevalence of HIV creates a population particularly vulnerable to opportunistic ocular infections.⁵These factors necessitate cautious antimicrobial stewardship. The emergence of antimicrobial resistance in ocular pathogens, including Staphylococcus aureus and Pseudomonas aeruginosa, demands judicious use of combination therapies. Balance the anti-inflammatory benefits of steroids against the risk of masking progression or delaying healing in incompletely treated infections.
PRACTICE RECOMMENDATIONS
Establish microbiological diagnosis where possible before initiating therapy. In resource-limited settings, empirical treatment may be necessary, but culture

should be attempted in severe cases.
Then begin with appropriate antimicrobial monotherapy based on likely pathogens and local resistance patterns. Avoid steroid use until effective antimicrobial therapy is established for at
least 48-72 hours.³ Consider adjunctive corticosteroids in severe cases with significant inflammation, particularly those with deep stromal involvement or risk of perforation. Monitor closely for signs of treatment failure or complications. Ensure
Offer Neuroprotection1
proper follow-up and referral pathways to specialist care when available, particularly for complex cases or those not responding to initial therapy.
References available on request.


CLINICAL | GASTROENTEROLOGY
C Beyond the stigma: Piles care
Haemorrhoidal disease represents one of the most common proctological conditions encountered in clinical practice.
ONTEMPORARY UNDERSTANDING RECOGNISES
haemorrhoids as the symptomatic enlargement and displacement of normal anal cushions rather than simple varicose veins.¹ This article reviews current evidence-based management strategies for healthcare professionals. Modern haemorrhoidal pathophysiology centres on the 'sliding anal canal lining' theory. Normal anal cushions are vascular structures in the
right anterior, right posterior, and left lateral aspects of the anal canal. Disease develops through deterioration of supporting tissues, leading to venous dilatation, vascular thrombosis, and collagen degeneration.¹ Risk factors include straining during defaecation, prolonged sitting, chronic constipation, obesity, and pregnancy.² The condition is classified into four grades based on prolapse degree and reducibility.
Fast, clinically proven, with natural ingredients for the relief of haemorrhoids (piles) symptoms1
ActiProct® Gel works within 60 seconds to relieve the pain & discomfort caused by Grade I & II haemorrhoids (piles)1
5-way action to effectively: 1
Relieve haemorrhoids & anal discomfort
Reduce inflammation
Relieve pain
Soothe itch
CONSERVATIVE MANAGEMENT
First-line management focuses on lifestyle modifications and dietary interventions. The American Society of Colon and Rectal Surgeons (ASCRS) 2024 guidelines provide strong recommendations for dietary modification and increased fibre intake as primary therapeutic measures.³ Patients require counselling on proper bowel habits, avoiding excessive straining, and limiting toilet time. Fibre
supplementation demonstrates significant efficacy in reducing symptoms and bleeding.⁴ Bulk-forming laxatives are recommended when hard stools persist despite lifestyle changes. Phlebotonics may be considered for both acute and chronic disease, reducing bleeding, pruritus, discharge, and leakage.⁴ Sitz baths remain valuable adjunctive therapy, helping relax sphincter muscles and decrease inflammation.
TOPICAL THERAPEUTIC OPTIONS



Protect from irritation & friction during toilet visits









AskforProct!

Topical treatments encompass formulations containing analgesics, anaesthetics, steroids, venotropics, antiseptics, and emollients.⁵ These provide short-term symptom relief, though evidence varies considerably. Hydrocortisone, frequently included in topical preparations, reduces inflammation and swelling. However, systematic reviews highlight limited high-quality evidence supporting topical hydrocortisone as first-line treatment.⁵ Guidelines recommend short-term use only due to potential local side effects with prolonged application.
Antiseptic agents have been incorporated into preparations to prevent secondary infection. While triclosan-coated sutures demonstrate efficacy in reducing surgical site infections,⁶ specific evidence for topical antiseptic use in non-surgical haemorrhoidal management remains limited.
INTERVENTIONAL MANAGEMENT
For patients failing conservative measures, rubber band ligation (RBL) is the most effective office-based treatment for symptomatic Grade I-II haemorrhoids and select Grade III cases.³ This represents a strong guideline recommendation supported by moderate-quality evidence.
Surgical intervention is reserved for Grade III-IV haemorrhoids failing conservative and office-based treatments. Excisional haemorrhoidectomy remains the gold standard, offering excellent long-term results but with significant postoperative pain.⁷ Doppler-guided haemorrhoidal artery ligation provides reduced pain but variable recurrence rates.⁷
CONCLUSION
Contemporary haemorrhoidal management follows structured, evidence-based approaches beginning with lifestyle modifications and progressing through office-based procedures to surgical intervention when indicated. While topical treatments remain popular for symptom relief, their evidence base is limited, requiring judicious short-term use only. Prioritise patient education regarding lifestyle modifications and appropriate care escalation when conservative measures prove insufficient.
References available
Beyond the Burn: Managing GERD in Complex Patients

Dr Peter Barrow
MBBCh (Wits); DCH (SA); FCP (SA); Cert. Gastro (SA)
Date: 17 November 2025
Time: 7pm
Topic: Beyond the Burn: Managing GERD in Complex Patients
Speaker: Dr Peter Barrow
CLICK TO REGISTER: https://bit.ly/AdcockIngramWebinar17Nov25
Dr Barrow is a consultant gastroenterologist trained at the University of Witwatersrand, with a special interest in interventional endoscopy including double balloon endoscopy (DBE) and endoscopic ultrasound (EUS). He has extensive clinical and research experience in inflammatory bowel disease (ulcerative colitis and Crohn’s disease), celiac disease, oesophageal motility disorders and GERD. He is a well recognised speaker and respected by his peers. Dr Barrow readily shares his practical and clinical expertise and often engages in clinical meetings and elements. Dr Barrow currently serves as an Honorary Lecturer at School of Clinical Medicine,

Witwatersrand University and has numerous achievements during his career, amongst which are the following:
- He was involved as an investigator in several clinical trials and is currently working on three new clinical trials on Crohn’s Disease and Ulcerative Colitis
- Presented at International congresses, as recently as International Association of Gastroenterology in Cape Town, Aug 2019 on: “Evaluation of Pancreatic Cystic lesions. What is state of the art?”


CLINICAL | DERMATOLOGY
Healing beyond the surface: Care for burn scar patients
Burn injuries represent a significant healthcare burden globally, with thousands requiring hospital admission annually.
WHILE ADVANCES IN acute burn care have significantly improved survival rates, the long-term management of burn scars remains a complex challenge that requires comprehensive understanding of scar pathophysiology and evidence-based treatment approaches.
PATHOPHYSIOLOGY OF BURN SCAR FORMATION
Burn scar formation represents a complex cascade of biological processes that begins immediately following thermal injury. The process unfolds through three distinct yet overlapping phases: the acute inflammatory phase, the proliferative phase, and the remodelling phase.1 During the acute inflammatory phase, which typically lasts 3-5 days post-injury, there is immediate activation of the coagulation cascade and recruitment of inflammatory cells. Pro-inflammatory cytokines including tumour necrosis factor-alpha (TNF- α), interleukin-1 beta (IL-1β), and interleukin-6 (IL-6) orchestrate the initial response, while anti-inflammatory mediators such as interleukin-10 (IL-10) and transforming growth factor-beta 3 (TGF-β3) attempt to modulate excessive inflammation.1
The proliferative phase, extending from approximately day three to week three post-injury, is characterised by fibroblast activation and transdifferentiation to myofibroblasts. This process is largely mediated by transforming growth factorbeta (TGF-β) signalling, which promotes excessive deposition of type I and III collagen.1,2 The balance between collagen synthesis and degradation becomes disrupted, with matrix metalloproteinases (MMPs) playing crucial roles in determining final scar quality. The remodelling phase, which can extend for months to years, involves gradual reorganisation of collagen fibres and scar maturation. Nerve growth factor (NGF) and neuropeptides including substance P and calcitonin gene-related peptide (CGRP) contribute to nerve remodelling within the scar tissue, often resulting in altered sensation and pain sensitivity.1
CLASSIFICATION AND CLINICAL PRESENTATION
Burn scars present with varying degrees of severity depending on multiple factors including burn depth, anatomical location, patient age, and genetic predisposition. Superficial burns typically heal with minimal scarring, while deep partial-thickness and full-thickness burns frequently result in significant scar formation. Hypertrophic scars represent pathological scarring characterised by excessive collagen deposition within the boundaries of the original wound. These scars are raised, firm, and often associated with pruritus and pain.
Keloid scars extend beyond the original wound boundaries and are more common in certain ethnic populations, particularly those of African or Asian descent.2
Contracture scars pose particular challenges, especially when they cross joint lines or involve functionally important areas such as the hands, face, or neck. These scars can significantly impact quality of life through both functional limitations and psychological distress.
PREVENTION STRATEGIES
Early intervention remains the cornerstone of burn scar prevention. Optimal wound care during the acute phase, including appropriate debridement, infection control, and maintenance of a moist wound environment, significantly influences final scar quality.3 Pressure therapy using custom-fitted garments has long been considered standard care for prevention of hypertrophic scarring, particularly in areas amenable to compression. The mechanism is thought to involve reduction of tissue oxygenation and modulation of collagen synthesis. However, patient compliance remains challenging due to discomfort and the requirement for prolonged wear.3
Silicone-based products, including gels and sheets, have emerged as first-line preventive treatments with robust clinical evidence supporting their efficacy. Multiple systematic reviews have demonstrated that silicone products significantly reduce scar height, pigmentation, and pliability compared to standard care.4 The exact mechanism remains unclear but is thought to involve tissue hydration and modulation of the local inflammatory response.
THERAPEUTIC INTERVENTIONS
For established burn scars, treatment options range from topical therapies to surgical intervention. The choice of treatment depends on scar characteristics, patient factors, and functional impact.
TOPICAL TREATMENTS
Corticosteroids remain the gold standard for treating hypertrophic scars, with intralesional triamcinolone acetonide being most commonly used. Response rates vary from 50-100%, with combination approaches using 5-fluorouracil or botulinum toxin showing enhanced efficacy.5 Topical corticosteroids may be beneficial for superficial scars but have limited penetration in mature scar tissue. Emerging evidence supports the use of botanical oils in scar management. Rosehip oil has demonstrated particular promise, with clinical studies showing significant improvements in scar appearance, pigmentation, and healing time compared to conventional treatments.6 A randomised controlled trial involving 60
burn patients found that rosehip extract ointment resulted in faster wound healing (7.53 days versus 11.83 days) and higher patient satisfaction compared to silver sulfadiazine.6 The mechanism is attributed to the oil’s high content of essential fatty acids, retinoids, lycopene, and betacarotene, which support tissue regeneration and reduce hyperpigmentation. Vitamin E supplementation, either topical or oral, has shown inconsistent results in clinical studies. While some research suggests potential benefits when combined with other treatments, up to one-third of patients experience skin irritation or contact dermatitis with topical vitamin E.7 Current evidence does not support vitamin E monotherapy for burn scar management.
Silicone-based products,including gelsandsheets, haveemergedas first-linepreventive treatments with robust clinical evidencesupporting theirefficacy
ADVANCED THERAPEUTIC MODALITIES
Laser therapy has revolutionised burn scar treatment, with pulsed dye lasers (PDL) and fractional carbon dioxide lasers showing significant efficacy in improving scar texture, pigmentation, and pliability. Optimal results are typically achieved when laser treatment begins at least 12 months postinjury, allowing for initial scar maturation.5 Microneedling has gained popularity as an adjunctive treatment, particularly when combined with topical therapies or plateletrich plasma (PRP). The controlled microinjuries stimulate collagen remodelling and enhance penetration of topical treatments.5 Emerging molecular therapies targeting specific pathways in scar formation show promise but remain largely experimental. Approaches targeting TGF-β/SMAD signalling pathways using nanogels, RNA interference, and small molecules are under investigation but require more robust clinical trials.8
HOLISTIC MANAGEMENT APPROACH
Effective burn scar management requires a multidisciplinary approach addressing both physical and psychological aspects of care. Patient education regarding realistic expectations, treatment timelines, and the importance of compliance with preventive
measures is crucial. Psychological support should be integrated early in the care pathway, as burn scars can significantly impact self-esteem, body image, and social functioning. Studies have shown that patients with visible burn scars have higher rates of depression, anxiety, and post-traumatic stress disorder compared to the general population. Regular follow-up allows for early identification of problematic scarring and timely intervention. Scar assessment tools such as the Patient and Observer Scar Assessment Scale (POSAS) provide standardised evaluation methods that facilitate clinical decision-making and research.
FUTURE DIRECTIONS
The field of burn scar management continues to evolve with advancing understanding of wound healing biology and scar formation mechanisms. Personalised medicine approaches incorporating genetic factors that influence scarring propensity may allow for more targeted interventions. Bioengineering approaches, including stem cell therapy and tissue engineering, hold promise for the future. However, translation from laboratory to clinical practice requires extensive validation and safety assessment. The development of objective, quantitative assessment tools using imaging technologies and biomarkers will enhance our ability to evaluate treatment efficacy and guide therapeutic decisions.
CONCLUSION
Burn scar management remains a complex clinical challenge requiring comprehensive understanding of scar biology and evidence-based treatment approaches. While significant advances have been made in both prevention and treatment strategies, optimal outcomes require early intervention, appropriate patient selection, and individualised treatment plans.
The growing evidence base supporting topical treatments, particularly siliconebased products and botanical oils such as rosehip oil, provides healthcare professionals with effective, accessible treatment options. However, more rigorous clinical trials are needed to establish optimal treatment protocols and combinations. Success in burn scar management ultimately depends on a multidisciplinary approach that addresses not only the physical aspects of scarring but also the psychological and social impacts on patients’ lives. Continued research into the molecular mechanisms of scar formation will undoubtedly lead to more targeted and effective therapeutic interventions in the future.
References available on request.





















Spring allergic disease: connecting allergic rhinitis to asthma for a better outcome
Allergic rhinitis, often dismissed as a mere inconvenience, represents one of the most prevalent allergic conditions worldwide, affecting up to 50% of the population in certain regions.
To view a CPD-accredited recording of this talk, please visit https://event. webinarjam.com/go/replay/1085/q7647f6l7h1mqux6wck

RECENT INSIGHTS FROM Dr Eva Södergren’s comprehensive webinar reveal the critical importance of recognising and properly managing this condition, particularly its intricate relationship with asthma. Dr Södergren, a PhD in nutrition with over 25 years of experience and 18 published papers in food allergy and clinical nutrition, currently serves as senior manager in Allergy, Global Medical and Scientific Affairs at Thermo Fisher Scientific, where she has worked for 14 years.
THE HIDDEN BURDEN OF ALLERGIC RHINITIS
The clinical significance of allergic rhinitis extends far beyond nasal symptoms. Research demonstrates that patients with allergic rhinitis are three times more likely to develop asthma, establishing a clear connection between upper and lower respiratory tract allergic diseases. This relationship is particularly concerning when considering that uncontrolled moderate to severe allergic rhinitis can significantly worsen asthma control, leading to increased morbidity and healthcare utilisation.
The economic and clinical implications are substantial. Studies indicate that proper diagnosis and management of allergic rhinitis can reduce asthma-related hospital visits by up to 50%, highlighting the critical importance of early intervention and appropriate treatment strategies.¹ This reduction in hospital admissions not only improves patient quality of life but also represents significant cost savings for healthcare systems.
Molecularallergology representsthe next frontier in allergicdisease diagnosis,providing deeperinsights bydistinguishing primarysensitisation fromcross-reactivity patterns
DIAGNOSTIC CHALLENGES IN CLINICAL PRACTICE
One of the most pressing issues in allergic rhinitis management is the underutilisation of diagnostic testing in primary care settings. A recent US survey revealed that 89% of patients with rhinitis symptoms
are not tested for allergic triggers, leading to widespread reliance on symptomatic treatment without addressing underlying causes.² This approach often results in suboptimal outcomes and missed opportunities for targeted interventions.
The challenge lies in differentiating allergic rhinitis from non-allergic and infectious rhinitis, as these conditions present with overlapping symptoms. Case history alone provides only 50% diagnostic accuracy, emphasising the need for objective testing methods to guide clinical decision-making.³
THE POWER OF SPECIFIC IGE TESTING
Specific IgE blood testing represents a transformative tool in allergic disease diagnosis. When combined with comprehensive case history, this testing method can improve diagnostic accuracy from 50% to an impressive 90%. This dramatic improvement in diagnostic certainty enables healthcare professionals to move beyond symptomatic management towards precision medicine approaches.
The stepwise diagnostic approach begins with detailed case history, progresses to specific IgE testing for whole allergens and allergen components, and may advance to molecular allergology for complex cases. This systematic methodology ensures accurate identification of allergic triggers while optimising resource utilisation.
MOLECULAR ALLERGOLOGY: ADVANCING PRECISION DIAGNOSIS
Molecular allergology represents the next frontier in allergic disease diagnosis, providing deeper insights by distinguishing primary sensitisation from cross-reactivity patterns. This sophisticated approach is particularly valuable in polysensitised patients, where multiple allergen sensitivities can complicate treatment decisions. For healthcare professionals dealing with complex allergic presentations, molecular allergology offers the ability to identify genuine allergen triggers versus cross-reactive proteins. This distinction is crucial for developing effective avoidance strategies and determining appropriate immunotherapy candidates.
CLINICAL IMPLICATIONS FOR PATIENT MANAGEMENT
Early and accurate diagnosis of allergic rhinitis enables several clinical benefits. Firstly, identification of specific allergens allows for tailored avoidance strategies, reducing exposure to triggering substances. Secondly, precise diagnosis facilitates appropriate selection of allergen-specific

immunotherapy, which can provide longterm disease modification rather than mere symptomatic relief.
The clinical approach should particularly focus on children with repeated wheezing episodes and individuals demonstrating polysensitisation to multiple allergens. These populations are at heightened risk for developing persistent asthma and require careful monitoring and management.
TREATMENT OPTIMISATION AND PATIENT EDUCATION
Beyond diagnostic accuracy, successful allergic rhinitis management requires attention to treatment delivery and patient education. Many patients receive suboptimal benefit from medications due to incorrect administration techniques. For instance, proper use of intranasal corticosteroids, including correct positioning, technique, and timing, significantly impacts treatment efficacy. Regular follow-up visits are essential for monitoring disease progression, assessing treatment response, and adjusting management plans accordingly. This is particularly important in paediatric patients, where sensitisation patterns may change as children grow and develop.
ADDRESSING
HEALTHCARE SYSTEM CHALLENGES
Several barriers limit optimal allergic rhinitis management in clinical practice. Accessibility and cost of specific testing remain significant concerns, particularly in resource-limited settings. Additionally, the lack of consistent diagnostic pathways across different healthcare systems creates variability in patient care quality.
Healthcare professionals must advocate for improved access to diagnostic testing while working within existing constraints. This may involve strategic use of testing
resources, focusing on patients with severe symptoms, poor treatment response, or suspected multiple sensitisations.
FUTURE DIRECTIONS AND RECOMMENDATIONS
The integration of specific IgE testing and molecular allergology into routine clinical practice represents a critical advancement in allergic disease management. Enhanced communication between laboratory and clinical professionals ensures precise testing selection and appropriate interpretation of results, particularly in complex or multisensitised patients.
Healthcare systems should consider developing standardised pathways for allergic rhinitis diagnosis and management, incorporating evidence-based testing strategies and treatment protocols. This systematic approach can improve patient outcomes while optimising resource utilisation.
CONCLUSION
The relationship between allergic rhinitis and asthma represents a critical clinical connection that demands attention from healthcare professionals. Through proper diagnostic testing, particularly specific IgE measurement and molecular allergology, clinicians can move beyond symptomatic management towards precision medicine approaches that address underlying disease mechanisms. The evidence clearly demonstrates that early and accurate diagnosis of allergic rhinitis leads to improved asthma control, reduced healthcare utilisation, and enhanced patient quality of life. As healthcare professionals, recognising and acting upon this connection represents an opportunity to significantly impact patient outcomes while contributing to more efficient healthcare delivery.

Fascinating webinar by Dr Kobus Roux sheds light on the brain and behaviour
Dr Roux's webinar, entitled ‘The Addicted Brain - Part 1’, was sponsored by Adcock Ingram. During the talk, he offered a comprehensive exploration of addiction as an inherent function of the human brain, demonstrating how its evolutionary mechanisms are predisposed to addictive behaviours.
To view a CPD-accredited recording of this talk, please visit http://bit.ly/48bkpMu Please inform John.Woodford@media24.co.za once you have watched the webinar, including your name, surname and professional registration number.
THROUGHOUT THE WEBINAR,
Dr Roux detailed the relationship between the brain's reward system, addiction, and various mental health disorders. Dr Roux began by emphasising that the human brain is fundamentally structured to engage in addictive behaviour. This wiring stems from evolutionary adaptations essential for survival, such as the pursuit of food and shelter, which were driven by the brain's reward system.
The primary neurotransmitter involved in the reward system is dopamine, which reinforces behaviours by triggering a sense of pleasure and motivates repetition of those actions. In primitive conditions, the push-and-pull dynamic of hunger (pain) and feeding (pleasure) helped ensure survival.
As the discussion shifted to the modern context, Dr Roux explained that addictive substances and activities exploit this reward system by providing significantly higher dopamine releases compared to natural behaviours. He cited studies showing
that substances such as cocaine can produce dopamine surges many times higher than those from typical stimuli like eating or sex. This disproportionate reward often leads to the neglect of normal, healthy activities, which can manifest as passivity and dependency. Importantly,
Dr Roux highlighted the brain's tendency to seek balance between pleasure and pain. Persistent exposure to extraordinary pleasure from substances or behaviours reduces sensitivity to pleasurable stimuli and heightens sensitivity to pain, a phenomenon central to understanding addiction.
Treatment approaches for addiction were a significant focus. Dr Roux underscored that the bedrock of treating any addictive disorder is abstinence, which allows the brain to reset its reward thresholds. However, he advocated for a holistic, stepwise approach that extends beyond mere detoxification. This includes gathering detailed behavioural data,
setting treatment objectives, addressing addiction-related problems, and employing abstinence as a foundation. Longterm recovery involves psychotherapy, mindfulness practices, routine building, and the discovery of alternative sources of reward, such as exercise or creative outlets, to re-engage the brain's reward system positively.
Dr Roux explained that addiction is rarely an isolated diagnosis. Most substance use disorders involve a dual diagnosis, wherein addiction coexists with other psychiatric conditions such as anxiety, depression, or schizophrenia. He also highlighted compelling research linking metabolic syndromes like insulin resistance to addictive behaviours and psychiatric disorders. For example, therapeutic interventions targeting metabolic factors (eg, ketogenic diets) show promise in treating major depressive disorder and even schizophrenia. The webinar also explored societal shifts in addictive behaviours, with

Dr Roux illustrating how modern phenomena such as screen addiction, obesity, and compulsive shopping manipulate the brain's natural inclinations.
He cautioned against viewing these behaviours as merely lifestyle choices, instead advocating their recognition as clinical concerns. In terms of pharmacological progress, Dr Roux mentioned advancements in treating co-occurring psychotic disorders and substance use disorders with thirdgeneration antipsychotics, specifically those targeting dopamine D3 receptors. He concluded by reiterating the need for integrated approaches that consider addiction's complex interplay with biological, psychological, and societal factors.
Overall, Dr Roux's presentation comprehensively framed addiction as a natural yet hijacked process of the brain's reward system, encouraging a nuanced and multifaceted approach to management and treatment.
Dawn after the darkness: Topical therapeutic options for pigmentation
Dr Irshad Essack’s recent webinar presentation provided healthcare professionals with a comprehensive overview of contemporary approaches to managing pigmentation disorders, with particular emphasis on melasma and post-inflammatory hyperpigmentation (PIH).
HIS EVIDENCE-BASED discussion highlighted the critical importance of understanding melanogenesis pathways and implementing sequential therapeutic strategies for optimal patient outcomes.
UNDERSTANDING THE BIOCHEMICAL FOUNDATION
The presentation emphasised that effective pigmentation management begins with understanding the complex biochemical pathways underlying melanogenesis. Dr Essack detailed how tyrosinase enzymatic reactions, in conjunction with copper ions, drive melanin production through multiple molecular pathways. Hormonal influences, particularly oestrogen and melanocytestimulating hormone, play regulatory roles that must be considered when developing treatment protocols. Post-inflammatory pathways frequently exacerbate pigmentation disorders, necessitating the integration of anti-inflammatory agents into treatment regimens. This understanding forms the foundation for targeted therapeutic approaches that address both the underlying biochemical processes and inflammatory components contributing to pigmentation disorders.
CLINICAL CONDITIONS AND DIAGNOSTIC CONSIDERATIONS
Dr Essack’s presentation focused primarily on two prevalent conditions affecting diverse patient populations. Melasma, a common facial hyperpigmentation disorder, results from complex interactions between hormonal changes, sun exposure, and inflammatory processes. The condition requires careful diagnostic assessment using clinical evaluation, dermoscopy,
and occasionally tissue biopsy for complex cases. Post-inflammatory hyperpigmentation, increasingly recognised as “acne-induced hyperpigmentation,” occurs following skin injury or inflammatory conditions including acne, eczema, or physical trauma. Dr Essack emphasised the importance of accurate diagnosis to guide appropriate therapeutic selection and patient counselling regarding realistic treatment expectations.
The presentation also addressed exogenous ochronosis, a potential complication of chronic hydroquinone use presenting as greyish skin discolouration, and drug-induced pigmentation disorders commonly associated with hydroquinone misuse, antiretrovirals, anti-epileptics, and NSAIDs.
EVIDENCE-BASED THERAPEUTIC APPROACHES
Hydroquinone: The gold standard with limitations
Dr Essack positioned hydroquinone as the benchmark treatment for hypermelanosis while emphasising its limitations and potential complications. Clinical evidence supports its efficacy, but careful patient selection and monitoring are essential due to risks including cytotoxicity and ochronosis development. Best practice protocols limit hydroquinone use to 2–3 months, typically within triple combination therapy incorporating a retinoid and corticosteroid. Following induction therapy, patients require transition to non-hydroquinone maintenance agents to sustain therapeutic benefits while minimising adverse effects.
Alternative depigmenting agents
The presentation highlighted several
evidence-based alternatives offering comparable efficacy with improved safety profiles. Cysteamine emerges as a particularly promising non-hydroquinone option, modulating tyrosinase activity while providing antioxidant benefits. Head-tohead trials demonstrate comparable efficacy to hydroquinone with fewer side effects, enabling long-term maintenance therapy.
Azelaic acid represents another valuable therapeutic option, particularly for patients with contraindications to hydroquinone. Its safety profile during pregnancy and lactation, combined with efficacy in treating both melasma and acne-induced hyperpigmentation, makes it especially valuable for specific patient populations.
Retinoids and adjunct therapies
Tretinoin and other retinoids accelerate keratinocyte turnover, disperse melanosomes, and enhance penetration of other depigmenting agents. Their safety profile permits long-term use under appropriate supervision during maintenance phases following initial induction therapy.
Adjunct agents including niacinamide provide anti-inflammatory benefits and barrier repair support, while vitamin C offers stabilising and depigmenting properties when incorporated into customised formulations. These agents enhance treatment outcomes while supporting overall skin health.
CORTICOSTEROIDS: CONTROLLED INFLAMMATION MANAGEMENT
Topical corticosteroids serve a specific role in controlling inflammation and improving treatment adherence within combination therapies. However, Dr Essack emphasised their limitation to short-duration use

to prevent complications including skin atrophy, telangiectasia, and paradoxical steroid-induced pigmentation or rosacea development.
SEQUENTIAL THERAPY PROTOCOLS
The presentation strongly advocated for sequential therapy approaches, transitioning from aggressive induction therapy to safer maintenance protocols. This strategy maximises therapeutic benefits during initial treatment phases while minimising longterm complications through appropriate agent rotation and de-escalation.
SUN PROTECTION: THE THERAPEUTIC CORNERSTONE
Dr Essack emphasised that broad-spectrum sunscreens with SPF 50, preferably tinted formulations containing iron oxide, form the cornerstone of both prevention and treatment protocols. These products provide essential protection against high-energy visible light, which contributes significantly to pigmentation disorders, particularly in higher Fitzpatrick skin types.
PATIENT-SPECIFIC CONSIDERATIONS
The presentation highlighted the importance of individualised treatment approaches based on patient-specific factors including Fitzpatrick skin type, hormonal status, and potential medication-induced pigmentation. Patients with pregnancy or lactation require alternative agents such as azelaic acid and niacinamide, avoiding hydroquinone and retinoids. Higher Fitzpatrick skin types (IV–VI) demonstrate increased susceptibility to post-inflammatory pigmentation and exogenous ochronosis, warranting particularly cautious agent selection and monitoring protocols.

The patient journey –a patient-centric approach to healthcare delivery
The patient journey is an entire sequence of events that begins when the patient first develops a need for clinical care and engages with the healthcare system.

THE PATIENT JOURNEY follows the patients’ steps as they navigate the healthcare system, from initial scheduling to treatment to continuous care. The future of healthcare involves understanding and optimising the patient’s ‘journey’, which is the entire process a person experiences when seeking and receiving healthcare. By mapping and analysing this journey, healthcare providers can identify areas for improvement, enhance patient satisfaction and ultimately deliver better and more person-centred care. This includes everything from initial awareness to ongoing care and engagement, encompassing all interactions with the health system.
WHY IS THE PATIENT JOURNEY IMPORTANT?
Each touchpoint of patient engagement, from visiting your website to checking in for an appointment, can help or hinder meeting patient needs. To remain competitive, it is vital to view the patient journey as central to improving experience and closing gaps through continuous listening and feedback. In recent years, patient experience has become a key focus of regulatory programmes and payment incentives. However, relying only on post-visit satisfaction surveys captures limited touchpoints and risks overlooking insights from the full journey.
A HOLISTIC VIEW
This is key to modernising and strengthening efforts to meet patient needs. By breaking down silos, blind spots and hidden challenges in the patient experience can be identified. From initial awareness to ongoing care, the journey spans every interaction across the health system.
WHAT FACTORS DRIVE A PATIENT TO CHOOSE YOUR ORGANISATION/PRACTICE?
1. Awareness – what factors trigger the patient’s need for care and how does the patient learn about your organisation? Quality rating and online reputation, Campaign programmes, community involvement and networking. Other factors: Referrals, coverage and benefits and Healthcare provider search.
2. Access – access to healthcare services, when, where and at a time the services are needed.
3. Service delivery – the holistic, quality and sustained service delivery.
4. Ongoing care – continuous care is important. The focus is early detection and intervention and future care at a primary care site.
THE ROLE OF HEALTHCARE PROFESSIONALS IN PATIENT CARE
Navigating the healthcare system can be overwhelming. From routine check-ups to chronic care or specialist advice, the journey involves many stages and professionals. Patients engage with GPs, specialists, allied health providers and nurses – each playing a role in making care
seamless, effective and supportive.
COLLABORATION
IS ESSENTIAL
In modern healthcare, collaboration among health professionals is key to achieving the best patient outcomes. The patient journey is rarely linear or isolated to just one practitioner. Instead, it involves a coordinated effort among GPs, specialists, other health professionals and nurses. This multidisciplinary approach ensures that patients receive the most comprehensive and personalised care possible. This approach ensures holistic care, continuity of care, Improved patient outcomes and patient empowerment. When healthcare teams educate and involve patients in their care it encourages them to take an active role in managing their health, leading to better long-term outcomes.
PATIENT
JOURNEY MAPPING
Patient journey mapping captures key moments across the journey, offering an outside-in view of the experience. It helps identify gaps, inconsistencies and pain points often missed in standard feedback, supporting optimisation and improved satisfaction. A journey map also provides a cross-functional view, engaging teams and stakeholders in understanding patient behaviours and attitudes.
You can illicit information like:
- Do patients understand the follow-up care instructions?
- Do patients easily navigate the patient portals?
USING PATIENT JOURNEY DATA
It is important to start collecting data and driving action along your patient journey.
1. Collect data on all touch points of the patient journey.
2. Understand your patients’ interaction with your organisation.
3. Understand the data.
4. Use the data you collect to drive specific actions and feed into processes is vital to creating a seamless patient journey.
WHO OWNS THE PATIENTS’ DATA?
This is a hot topic of discussion in healthcare information technology (HIT) realm.
Patient data ownership can be broken down into:
1. Ownership of the data, versus
2. Medical records; and the ability of the patient to access the data.
LEGAL SIDE TO DATA OWNERSHIP
In the US, the Health Insurance Portability and Accountability Act (HIPAA) privacy rule, patients’ data are protected and patients have privacy and security around the information. It means that the patients must give the healthcare organisation permission to share their data with other healthcare organisations.
However, after the patients are seen by providers and
their histories, laboratory work, clinical presentation and other information are documented in medical records that the provider creates, the provider or healthcare organisations become owners.
Ownership of data is a complicated beast. Although the legal ownership of medical records does lie with the patients, that matter is debatable. Rules are in place that allows patients to access their data whether they own it or not and newer rules allow patients to be highly engaged in their own healthcare by making use of interoperable data.
UNDERSTANDING THE ROLE OF DATA
AI is used to characterise patients with complex care pathways that other solutions miss. AI assists in predicting patients’ pathology earlier in their disease journey. This allows the patient to receive more timely and accurate treatment and improved outcomes.
AI use in the patient journey is an out-of-the-box solution that delivers a comprehensive market opportunity assessment, patient characterisation, diagnosis and treatment journey analysis.
In 2013, BMI committed to set up an International Panel of Patients, patient advocates and clinicians to help develop a strategy to advance the ‘Patient Revolution’ in healthcare.
The BMI project hopefully will add National and International efforts to improve the quality, safety, value and sustainability of health systems through realising the transformative potential of working in partnership with patients, families, communities and advocacy groups.
CO-PRODUCTION
Co-production is a form of patient-centred care where patients and families partner with healthcare providers (eg. hospitals, physicians, nurses) to produce health. Batalden et al. describe it as a service co-created rather than a product delivered.
Both co-production and shared decision-making (SDM) rely on mutual respect and trust. When patients feel valued and listened to, they are more likely to engage. Co-production supports patient-centred care by codesigning care with patient input, tailored to the individual. SDM is a communication approach for preference-sensitive decisions, empowering patients with the information needed to make choices aligned with their values. In Crossing the Quality Chasm, the National Academy of Medicine (formerly Institute of Medicine) emphasised patient-centred care and highlighted SDM as a means to achieve it.
CONCLUSION
To survive in today’s healthcare landscape, it is important to look at the patients’ journey aiming to improve the patient experience. Health systems need to embrace the vision of the patient journey that is anticipatory, preventive and wholly centred on continuously improving the experience of patients, families and communities.
AI in Healthcare: Medical Protection's framework for safer practice
The integration of artificial intelligence (AI) into healthcare represents one of the most significant technological advances in modern medicine, offering transformative potential for diagnosis, treatment planning, and patient monitoring.

HILE THE BENEFITS of AI are substantial, the adoption of AI technologies in clinical practice also introduces complex challenges surrounding consent, accountability, clinical responsibility, and the boundaries of professional judgement.
Recognising these emerging concerns, Medical Protection has developed a comprehensive AI Safer Practice Framework – a two-part guidance system specifically designed to help healthcare professionals navigate the safe and effective implementation of AI in clinical care while maintaining appropriate medicolegal protection.
Framework components: INFORMED and RECORDS
The framework comprises two complementary components that work together to ensure ethical, accountable, and well-documented AI integration:
• INFORMED: A process-oriented guide that supports real-time clinical decisionmaking with AI
• RECORDS: A documentation-focused approach that ensures transparency and
accountability in AI-assisted care.
The INFORMED component
INFORMED serves as a real-time decisionmaking tool that maintains essential clinician oversight throughout the AIassisted care process. The component focuses on:
• Preserving critical clinical judgement and expertise
• Encouraging collaborative decisionmaking between healthcare professionals and AI systems
• Minimising automation bias – the tendency to over-rely on algorithmic recommendations
• Ensuring AI use aligns with established ethical practices
• Supporting healthcare professionals in maintaining their professional autonomy while leveraging AI capabilities.
Dr Sarah Townley, underwriting policy lead at Medical Protection, said: “The adoption and integration of AI into clinical care will be transformational, introducing a wealth of opportunities, and of course some risks. “In medicine, AI can be used to support diagnosis, treatment planning,
EDITORIAL
EDITOR: Claire Rush McMillan
Claire.Rush@media24.com
NEWS WRITER: Nicky Belseck
Nicky.Belseck@media24.com
SUB-EDITOR: Gill Abrahams
EDITORIAL CONTRIBUTORS
Conrad Strydom, Prof Morgan Chetty
LAYOUT & DESIGN: Naresh Budraj
ADVERTISING EXECUTIVES
Anel du Plooy - Tel: 082 786 9517
Anel.duPlooy@media24.com
Cindy Riederer - Tel: 082 492 0229
Cindy.Riederer@media24.com
DISTRIBUTION & SUBSCRIPTIONS
Felicity Garbers
Email: felicity.garbers@media24.com
Update your details here: www.medicalacademic.co.za
PUBLISHING TEAM
General Manager: Dev Naidoo
Head of Content & Digital Strategy: Varushka Padayachi
Production Manager: Angela Silver
Group Art Director: David Kyslinger
CONTACT
Johannesburg Office
Building 13, The Woodlands Office Park, 20 Woodlands Drive, Woodmead, Sandton PO Box 784698, Sandton 2146 +27 11 867 6111
COVER PRICE
Medical Chronicle per issue R60.00 VAT Incl.
Published by Media24 B2B
Printed and bound by Novus PrintMontague Gardens, Cape Town
MEDIA24 MEDIA
and monitoring, leaving clinicians to deal with the complexity created by the blurring of boundaries when it comes to clinical responsibility, professional judgement, and legal liability. “We are proud to introduce the AI Safer Practice Framework –designed to help healthcare practitioners navigate the challenges that might be presented when using AI in medical practice, and ensure their clinical records support them in case of any medicolegal challenge.” Dr Ben White, cases team lead at Medical Protection, added: “INFORMED - the first part of our framework - is a real-time, processbased guide for using AI in clinical care. It supports clinician oversight, promotes collaborative decision-making, and reduces potential automation bias thereby avoiding over-reliance on algorithmic systems.
“The second part of the framework – RECORDS - is used for documenting AI-driven decisions. It captures clinical rationale, the role AI has played, and the clinician’s decision – crucial for transparency in audits, complaints, or legal reviews.”
CEO: Minette Ferreira
CFO: Lana Goliath
MEDIA24 CORPORATE
CEO MEDIA24: Raj Lalbahadur
CFO MEDIA24: Nelmarie Beyers
Unless previously agreed in writing, Medical Chronicle owns all rights to all contributions, whether image or text.
SOURCES: Gettyimages, supplied images, editorial staff. Articles are created with the assistance of artificial intelligence (AI) tools to aid in research and drafting. The content has been reviewed and edited by a human expert for quality and reliability. While precautions have been taken to ensure the accuracy of its contents and information given to readers, neither the editor, publisher, or its agents can accept responsibility for damages or injury which arise therefrom. All rights reserved. © Medical Chronicle. No part of this publication be reproduced, stored in a retrieval system or transmitted in any form or by any means, photocopying, electronic, mechanical or otherwise without the prior written permission of the copyright owners. Attention African readers: Please note that some products might not be available in your region and product names could vary. Please contact your local distributors, agents or pharmaceutical companies concerned for any discrepancies.

Including content generated by Medical Chronicle, Specialist Forum, Pharmacy Magazine and the SA Ophthalmology Journal.








For more information, please contact us:
Editor: Conrad.Strydom@newmedia.co.za
Key Account Managers:
Cindy.Riederer@newmedia.co.za | Tel: 082 492 0229
Anel.duPlooy@newmedia.co.za | Tel: 082 786 9517
/ Stay up to date
Be the first to receive email updates on all things CPD, keep abreast of latest industry revelations, and keep adding to your CPD point score.
/ Catch up on your webinars
Never miss a webinar with our replay channel.
/
Register
Register with your FREE CPD account for access to clinical and CPD approved content.
